
3 Examples of Computerized Cognitive Testing
Published: 17/05/2025 | 3 min read
Written by: Creyos
Cognitive assessments provide critical information throughout the patient journey. Regular evaluations can drastically improve patient care and outcomes, from strengthening diagnostic decisions to long-term monitoring for at-risk patients. By leveraging a modern assessment solution, like Creyos Health, clinicians can make evidence-based decisions and improve patient outcomes. This includes neurocognition testing, which supports clinicians in evaluating core brain functions efficiently and effectively. Here are a few ways computerized neurocognitive testing can be used, including examples of how and why they play a key role in modern healthcare practices.
58% of Neurologists Use A Low-Sensitivity Screener to Detect Dementia
What are the standard assessments neurologists are using today—and are there better tools? Download our ebook Advancing Dementia Diagnosis to learn more.
3 Ways to Use Neurocognitive Assessments in Clinical Practice
1. Supporting Diagnostic Decisions
Importance
Determining a diagnosis is often the first step to understanding what is going on with a patient and developing a treatment plan. For example, if a patient has concerns about cognitive decline or dementia, early detection and diagnosis are critical, and every delay in treatment impacts patient outcomes.
Current Methods
- Refer to specialist
- Screening tools (MMSE, MoCA, SLUMS, etc.)
- Self-reporting
Benefits of Modern Neurocognitive Assessments
Modern cognitive assessments offer a middle ground that addresses the challenges associated with traditional assessments that are either too time-consuming or not detailed enough. They do not replace clinical judgment or a neuropsychologist, but they can provide more detailed information than a screener or a self-report by assessing across a variety of cognitive domains and comparing patient results to an extensive normative database of age-matched cohorts.
2. Medication Management and Progress
Importance

Cognitive assessments are useful in ongoing care, as they can help track patient progress and therapy effectiveness. However, it is not common or practical to administer complete neuropsychological assessments at every point when a change in cognition is likely to occur. In addition, screening tools have limited forms, practice effects, and crude scoring, making it difficult to assess subtle changes over time. This means critical information is not being collected when it is most valuable, such as:
- When medication is taking effect
- As adjustments are being made to avoid side effects
- When a patient begins experiencing subjective improvements
Current Methods
- Subjective impressions from patients or caregivers
- Re-administration of screening tools
- Appointment follow-ups and interviews
Benefits of Computerized Neurocognitive Testing
Modern cognitive assessments provide a solution to these constraints. Clinicians can administer tests quickly and repeatedly, ensuring that cognitive data is collected at precisely the right time. Computerized testing allows for the random generation of test items on the fly, minimizing practice effects. Results can be automatically scored and compared to an extensive normative database that considers repeated testing and helps identify when a change from one time point to another is meaningful. Comorbid issues like mental health conditions and self-reported symptoms can be included in an integrated assessment flow to improve medication decisions and patient outcomes. With an efficient method for tracking cognition, clinicians can easily assess treatment efficacy, manage medications, and track overall status.
3. Monitor Cognition and Mental Health Over Time
Importance
Several neurological disorders result in a devastating reduction in cognitive function. Traditionally, long-term follow-up or ongoing tracking have not been readily available. It has been particularly challenging to track subtle changes that occur after treatment of a condition that may—or may not—have chronic effects.
Reduced cognitive function and poor mental health also predict adherence to treatment and reliance on unhealthy coping mechanisms such as substance abuse. As a result, by the time decline is uncovered, the patient’s condition has often reached a state where treatment will be more complicated than it would have been if cognitive issues had been caught early.
Current Methods
- Self-report questionnaires
- Waiting for patients to take action or re-engage with a physician
Benefits of Computerized Neurocognitive Testing
Modern cognitive assessments can automate long-term follow-up. Using solutions like Creyos Health in long-term follow-up scenarios can help determine:
- If a patient reporting memory decline actually performs worse in objective memory tests
- If the symptoms of a neurological condition, injury, or medication are getting worse or better
- If there are early warning signs that a decline in cognition could lead to complications, failing to follow recommendations, or unhealthy coping mechanisms
Automated assessments allow clinicians to quickly capture the patient’s status and help improve long-term outcomes. If early signs are detected, healthcare providers can proactively offer additional services or justify further treatment. If a patient’s treatment is working, long-term follow-up can help demonstrate that the treatment has lasting effects, which can serve as valuable data for communicating the benefits of treatment.
It also acts as a feedback loop for assessing whether other treatments might be effective. Mental health assessments or substance abuse questionnaires can also be included to capture a range of effects neurological conditions have.
Improving Cognitive Care with Modern Assessments
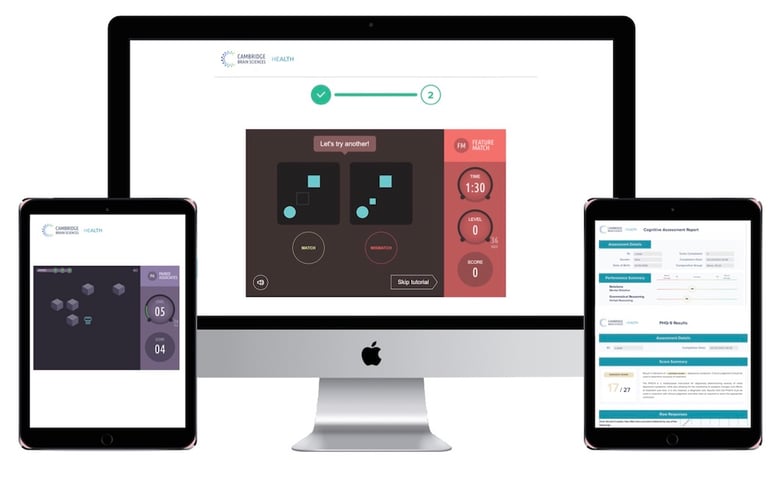
Implementing a modern neurocognitive assessment solution, like Creyos Health, ultimately provides clinicians with the tools they need to improve patient outcomes. Having a trusted and efficient method of testing cognitive function over time helps to:
- Improve clinical decision-making
- Detect meaningful change
- Drive data-based decisions
The comprehensive Creyos Health assessments allow neurologists to gain a more complete view of cognitive function, making it easy to quantify deficits and then track recovery and stability by establishing a personalized baseline.

