What is the IQCODE Measure for Cognitive Decline?
Published: 07/04/2025 | 5 min read
Written by: Mike Battista, Director of Science & Research
Globally, an estimated 57.4 million people were living with dementia in 2019, and this number is only projected to increase in the coming years (GBD 2019 Dementia Forecasting Collaborators, 2019). The cognitive decline that defines dementia can impact many aspects of a patient's daily life, making identification of everyday difficulties essential when it comes to choosing potential treatment options or planning for the future.
The self-report version of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE-SR), a questionnaire now available within Creyos Health, is the newest addition to the Creyos cognitive screening tests. It is designed to help clinicians assess subjective cognitive decline among older adults, and may aid in the early detection and diagnosis of Alzheimer's disease, other types of dementia, or other neurodegenerative diseases linked to cognitive decline.
What is the IQCODE?
The IQCODE is a 16-item screening tool designed for older adults that requires patients to answer simple questions pertaining to how they function within their daily lives. It was created by Anthony F. Jorm and colleagues in the 1980s, originally as a 39-question interview, but subsequent diagnostic accuracy studies and validation led to shorter versions that could be completed as questionnaires. The Creyos implementation is a condensed version of the IQCODE that stems from a 26-question variation. The short form version has nearly equal test accuracy, but requires less time from patients and is simpler for healthcare providers to interpret (see Jorm, 2004).
The IQCODE featured within Creyos Health is also completely self-reported (thus also known as the IQCODE-SR), eliminating the need for any dependence on other parties who may not be available when a patient visits the clinic or takes an assessment at home. The self-reported version also reduces informant factors, such as the informant’s mental health status, that can affect results. However, it can be completed with assistance when required (Jansen et al., 2008).
How does the IQCODE work?
Each question on the IQCODE asks patients to compare their present performance on an everyday task, such as remembering addresses and phone numbers, to how they would have performed on it 10 years prior. Answers are given on a 5-point scale ranging from “much improved” to “much worse,” with each response on the scale associated with a different number of points.

A patient’s score on the IQCODE is calculated by determining their average rating. The IQCODE scoring process adds up all individual item points and divides that number by 16, the total number of questions answered, so that the score represents average change across items. “Not much change” is represented by a score of 3, so any score above 3 means the patient indicated general decline in everyday mental tasks.
IQCODE reliability and validity
The IQCODE has high reliability and internal consistency. Its validity as a screening test has been established by showing that it correlates with traditional dementia screeners, objective testing, and future dementia risk. It also seems to be relatively unaffected by education and language, making it practical in diverse populations (see Jorm, 2004, for a review).
Jansen et al. (2008) found that the self-report version of the IQCODE has similar validity as the information version. Feasibility of administration in older adults is acceptable, though some individuals may fail to fill out the questionnaire when asked, especially if severe cognitive impairments are already present. As a result, the IQCODE-SR may be most useful when screening for signs of mild cognitive decline as early as possible.
Using the IQCODE to identify cognitive decline
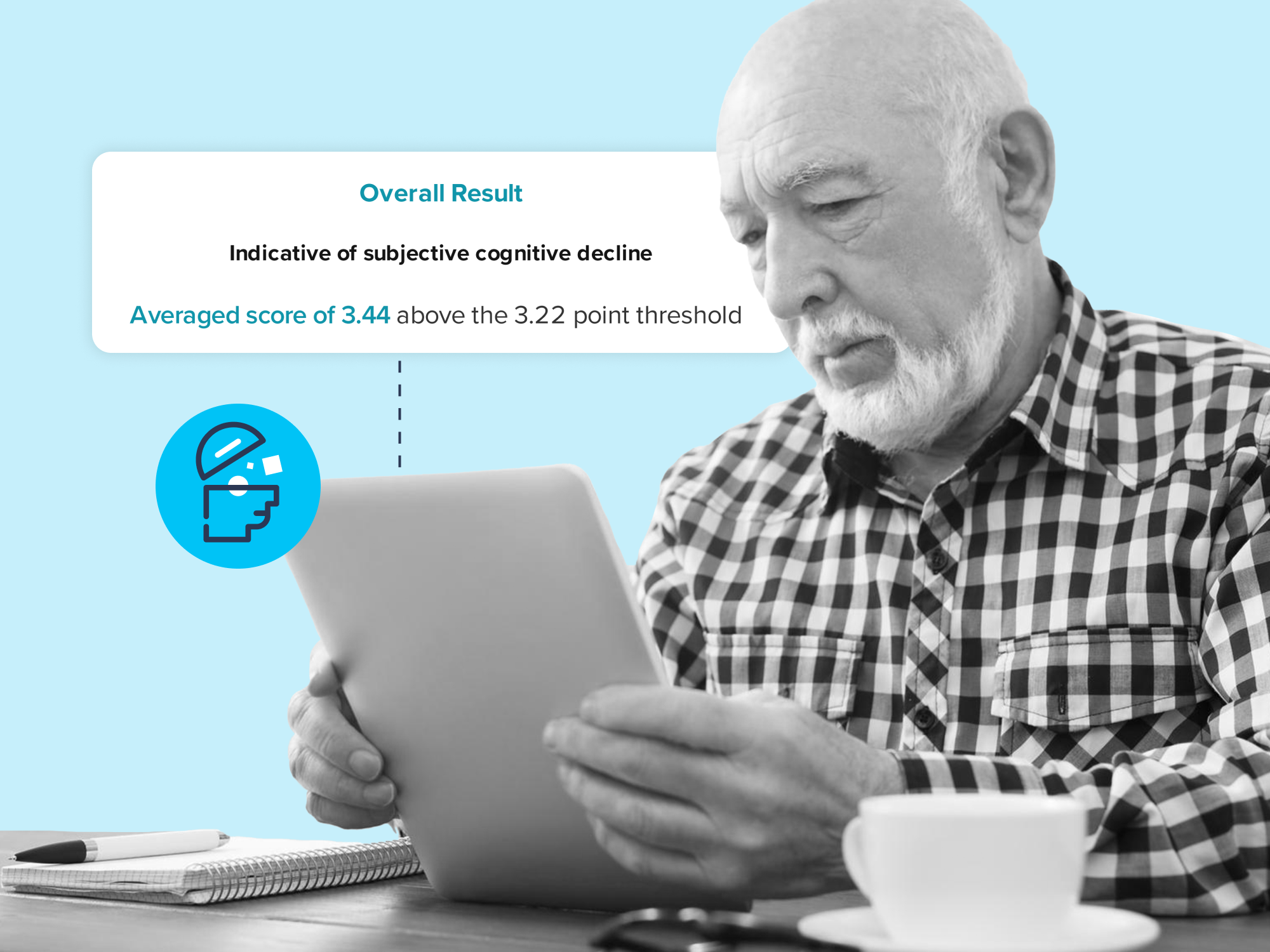
Examining the discriminative and predictive power of the IQCODE, Isella et al. (2006) found that the instrument is a valid clinical assessment for differentiating between healthy older adults and those with cognitive disturbances. An MCI diagnosis was unlikely for patients with IQCODE scores less than 3.22, so the Creyos version of the IQCODE sets a cutoff score of 3.22 for identifying subjective cognitive decline that requires longitudinal monitoring. However, higher scores indicate greater severity—scores greater than 3.45 are associated with a risk of transitioning from mild impairment to dementia within the following 2 to 3 years.
What role do subjective and objective cognitive decline measurements play in identifying mild cognitive impairment (MCI)?
Age and cognition are closely connected. Nearly 12% of adults over the age of 65 in the United States report subjective cognitive decline, according to the CDC. This decline is not only seen in terms of overall cognitive function, but across multiple cognitive domains, such as short-term memory, verbal ability, and reasoning. In fact, age is one of the strongest predictors of score on Creyos cognitive tests, with scores usually peaking around age 21 to 30 and then declining as age continues to increase (Nichols et al., 2021; Wild et al., 2018).
Understanding these cognitive changes is of utmost importance for clinicians working with elderly people. It has been projected by the World Health Organization that in less than 10 years, 1 in 6 people will be over the age of 60. According to the Alzheimer’s society, 5% to 8% of these people will suffer from dementia. Dementia refers to decline in cognition that is more severe than the drop associated with normal aging and severely impacts a person’s ability to live independently.
Mild cognitive impairment (MCI) is a condition that falls between normal age-associated impairment and dementia. It involves cognitive difficulties, disorientation, and difficulty communicating, without having a major impact on daily independent living. Subjective cognitive decline is a defining symptom of both dementia and MCI, and the IQCODE-SR allows practitioners to quantify subjective drops in cognition over the past 10 years. It can be used as part of a process for diagnosing and quantifying MCI or dementia, informing the subjective decline component of diagnostic criteria (e.g., the DSM 5 criteria for mild neurocognitive disorder include “concern of the individual, a knowledgeable informant, or the clinician”). The Creyos cognitive tasks may then be used to quantify objective impairment or decline, especially in high-risk individuals.
How to administer a computerized version of the IQCODE in Creyos Health
The IQCODE-SR is available as a questionnaire within Creyos Health. It can be completed on its own or within a protocol that includes any combination of cognitive assessments and questionnaires.
To include the IQCODE-SR in a Creyos Health assessment, simply click on the Questionnaires tab under Assessment Types when creating a protocol and then select the IQCODE. You may also select any other questionnaires or cognitive assessments to combine them all into one straightforward cognitive testing experience for your patients.
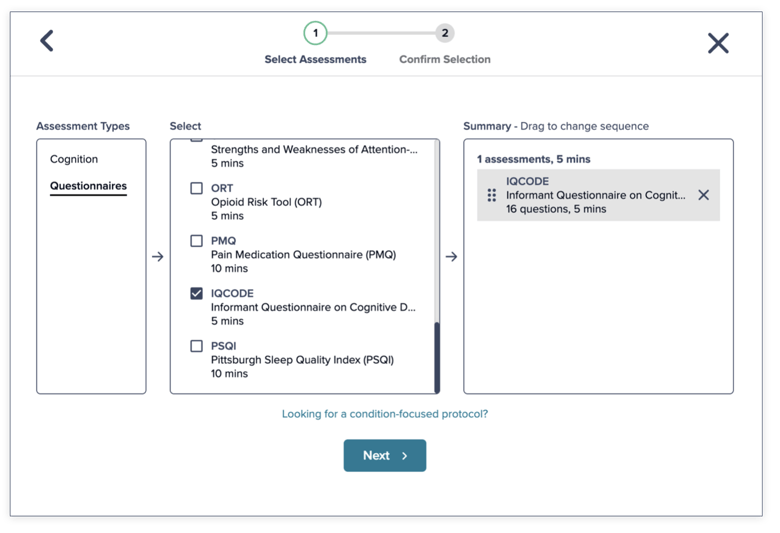
The Creyos Health version of the IQCODE can be completed either in healthcare settings or privately at home. It requires no special training to administer. The IQCODE can also be added to a Creyos Health schedule, allowing you to regularly send it automatically via email. Data collection is automatic and the results are scored instantly then added to an easy-to-interpret PDF report.
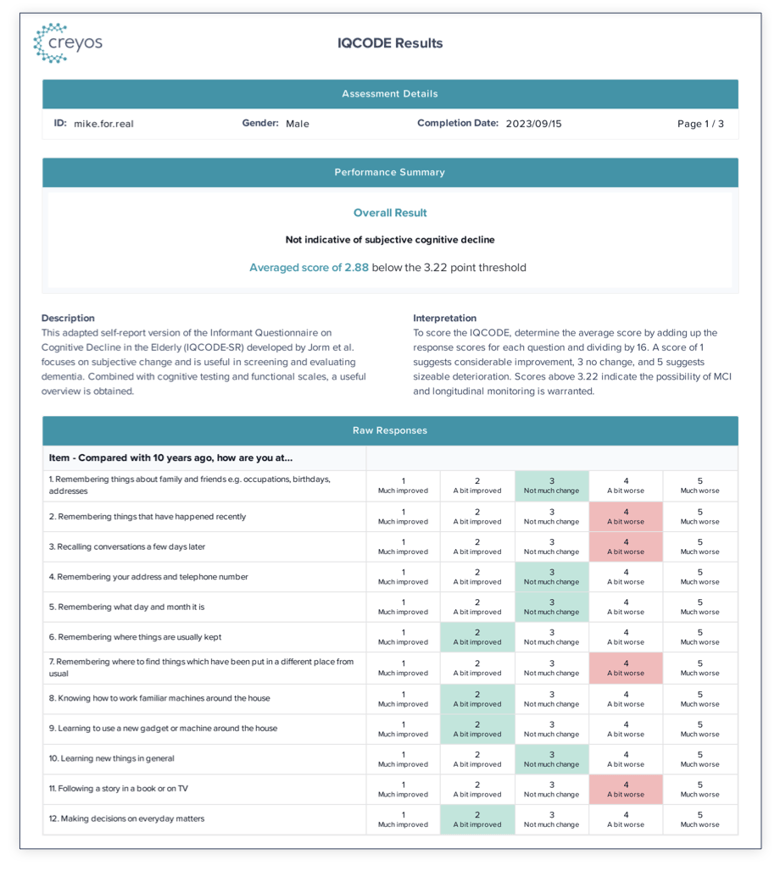
A report clearly displays results related to a patient's subjective decline. An overall result compares results to a research-based cutoff, and clinicians can see each response summarized as well. This allows primary care physicians to isolate areas of particular concern and conduct additional dementia testing or prepare a referral.
No patient login or registration are required in order to complete the questionnaire, making it incredibly simple for both patients and clinicians to benefit from this questionnaire and gain valuable information about the patient’s cognitive health.
For more detailed instructions on administering questionnaires within Creyos Health, please see our previous blog post on administering a computerized version of the PHQ-9.
Need more digital health questionnaires to measure cognitive decline in the elderly population?
If there are any questionnaires that you are using today as part of your practice that you would like to see become available in a computerized format within Creyos Health, please do not hesitate to let us know by commenting on this blog post or contacting us through email at help@creyos.com.
 Written by Mike Battista, Director of Science & Research at Creyos
Written by Mike Battista, Director of Science & Research at Creyos
Mike Battista specializes in brain health, cognition, and neuropsychological testing. He received his PhD in personality and measurement psychology at Western University in 2010 and has been doing fun and useful stuff in the intersection between science and technology ever since.

Reviewed by Sydni Paleczny, Staff Scientist
Sydni earned her MSc in Neurosciences at Western University under Dr. Adrian Owen. Her research explores neuropsychological outcomes after cardiac surgery, with interests in cognitive neuroscience, critical care, and brain health. At Creyos, she supports scientific validity, health technology, and ongoing research.
