
Continuity of Care: How to Retain Patients and Reduce Redundancy
Published: 09/07/2024 | 14 min read
Written by: Mike Battista, Director of Science & Research
Continuity of care is all about simplicity. It’s about improving patient experience by creating a system in which they get to see the same core team of healthcare providers, who become familiar with the patient’s health history and needs over time.
As far back as 2018, research has demonstrated an association between higher rates of continuity and reduced all-cause mortality (BMJ, BJGP). More recently, a 2023 systematic review of recent research identified a significant association between fragmented care and adverse outcomes of chronic illnesses (Nursing Open).
Continuous care requires a dedicated effort to ensure seamless and coordinated navigation through the intricate network of healthcare, beginning with the initial consultation and extending to subsequent follow-ups. Central to continuity of care is a focus on prioritizing patients’ specific needs, building trust, and nurturing understanding between those receiving treatment and the various health providers they interact with.
Today’s medical systems are complex, yet continuity of care aims to maintain patient safety by offering consistent standards in treatments over time. It represents an assurance to patients that despite potential confusion amidst referrals or changes during their course of treatment, they’ll experience a consistent and coherent approach that guides them toward improved health.
In this article, we’ll discuss the importance of continuity of care towards achieving superior quality in delivering medical services and offer practical perspectives on how to achieve it.
What Is Continuity of Care?
Continuity of care is the consistent and seamless provision of ongoing health care management to a patient over time, ensuring coordinated and high-quality treatment across various providers and settings.
The concept of continuity in care is pivotal to the management of patient health, giving patients a unified and methodical course throughout the complex terrain of medical services. Hand-in-hand with a patient-centered approach to care, establishing continuity is a dedication to enhancing patient treatment across various health settings (including family medicine, nursing, brain health, and more). The approach centers on safeguarding patient welfare while providing cost-efficient healthcare solutions.
Haggerty et al. (BMJ) identified three types of continuity in every discipline:
- Informational: The consistent use of collected information from the patient’s medical and personal history to make appropriate recommendations and decisions about current care.
- Management: A steady and progressing approach to managing the patient’s health concern that adapts to changing needs and situations.
- Relational: This is the core of the patient-provider connection. Relational continuity is about forming relationships with multiple providers that bridge past, present, and future. It can also involve establishing a reliable and trusting atmosphere through continued therapeutic engagement. While primarily focused on the patient, good continuity of care also supports caregivers and families.
For these three types of continuity to be achieved, there needs to be an understanding of each patient’s medical history paired with diligent communication efforts within the continuum of healthcare providers. Excellent notes and record-keeping (from both in-person consultations and telehealth services) are also key.
Together, these elements construct a robust framework dedicated to team-based strategies for managing patients’ cases and incorporating social support services into overall wellness plans—all aimed at achieving superior standards in healthcare provision.
Continuity of Care for Nurse Practitioners
Care continuity is particularly important in the settings that nurse practitioners occupy. Nurse practitioners are tasked with understanding their patients' needs and effectively communicating this information to physicians, specialists, and fellow nurses, making them a linchpin in successful continuity of care.
By effectively sharing detailed patient records and fostering an environment of trust, nurse practitioners contribute to several critical aspects, including:
- The safe transition of patients across different healthcare settings and professionals
- Coordinated and consistent delivery of healthcare services to patients
- Enhanced communication between members of the medical team
- Maintaining management consistency in treatment strategies and drug administration
- Interoperability between facilities (also supported by robust electronic records)
The uninterrupted continuum of management is vital for fostering improved outcomes for those under medical supervision while also enhancing their overall experience with the healthcare system.
When there’s steady interaction with either a single nurse practitioner or provider, it paves the way for better communication channels, which can lessen errors related to medical attention and heighten levels of contentment among those receiving care.
Continuity of Care in Brain Health
Maintaining continuity of care in the realm of brain health is crucial, as it guarantees that patients with neurocognitive conditions experience consistent and well-integrated health services throughout their rehabilitation process.
Particularly in the context of progressive conditions like dementia, reducing redundancy in care is critical as it can mean more timely care, better patient compliance, and less strain on patients and caregivers.
Neurocognitive conditions often require care from multiple providers like primary care providers, neurologists, therapists, and social workers. For patients dealing with dementia, traumatic brain injury, Parkinson’s disease, or any other neurocognitive condition, continuity of care is essential because it:
- Facilitates comprehensive management
- Ensures consistency in treatment and support
- Fosters trust and rapport
- Enables tailored and individualized care
- Aids in monitoring progress and adapting care as necessary
- Creates seamless transitions and care coordination
- Prevents gaps in care
For example, in one study following dementia patients, continuity of care was associated with lower rates of hospitalization, emergency department visits, testing, and health care spending (JAMA Intern Med). As another example, supporting patients transitioning from an acute care environment to community-based rehab facilities is an approach that can combat issues such as mobility constraints and helps avert social isolation by providing continual support.
Related: Discussing Cognitive Health: How to Talk About Cognitive Health Care With Patients
Continuity of Care in Mental Health
In the past 10+ years, emergency mental health visits for young people have more than tripled. But what happens once the patient is discharged? A recent study (Mental Health Research) explored the importance of continuity of care in follow-up appointments for young patients with diagnosed psychiatric conditions. It also touched on the challenges healthcare providers face in delivering that care.
A standout outcome from the above-mentioned study was that young people were at least three times more likely to attend the follow-up community appointment if they had already seen the designated clinician before discharge.
The results of this study point to important questions healthcare providers face today about how to address gaps in continuity. Potential solutions include being able to administer regular mental health questionnaires, improve continuity of reporting between care teams, track significant changes, and more.
Continuity of care in mental health could entail:
- A sustained and collaborative approach to meeting patients’ psychological and emotional requirements
- Emphasizing the availability of mental health services and identifying systemic obstacles
- Distributing pertinent information in a timely and efficient manner to collaborating providers
- Encouraging peer support and community services to improve the accessibility of care
Within the realm of mental health, maintaining uninterrupted care goes beyond healthcare professionals. It equally highlights services such as community groups, day centers, and other socially oriented organizations that offer consistency outside of a medical setting.
Advancing Dementia Diagnosis
Examples of Continuity of Care
Continuity of care involves all individuals in team-based care—from family physicians to specialists, support staff to caregivers, and beyond. Here are just a few examples of continuity of care practices that clinicians, nurse practitioners, neurologists, and mental health professionals can implement:
Nurse Practitioners
Nurse practitioners have an extremely active role in patient care and can enhance continuity of care in many ways, such as:
- Discharge planning: Nurse practitioners and nurses play a critical role in discharge planning by ensuring that patients and their caregivers understand their post-hospital or post-clinic care instructions, medications, and follow-up appointments. For example, a nurse might create a detailed discharge plan that outlines daily medication schedules and dietary restrictions to help patients manage their health at home.
- Facilitating care transitions: Nurses act as liaisons between different healthcare settings, such as from hospital to home care or rehabilitation facilities. For instance, a nurse might coordinate with home health services to ensure that a patient has the necessary medical equipment and support upon returning home.
- Post-discharge follow-up: Nurses conduct follow-up calls or visits to monitor patients' recovery progress and address any concerns or complications. For example, a nurse might call a patient a week after discharge to check on their adherence to the treatment plan and answer any questions they might have about their medications or symptoms.
Brain Health
Interdisciplinary teams comprising neurologists, rehabilitation specialists, and primary care providers embody the principle of continuity of care. If members of the team prioritize continuity of care, patients gain the benefits of collaborative plans, fewer redundant tests, and involvement of the right professionals at the right times.
- Collaborative care plans: Interdisciplinary teams develop comprehensive care plans to address the multifaceted needs of patients with conditions such as dementia, traumatic brain injury, or Parkinson’s disease. For example, a neurologist might coordinate with a rehabilitation specialist to create a tailored therapy regimen that enhances cognitive function and mobility.
- Reduction in redundant testing: By maintaining detailed and shared medical records, these teams can avoid unnecessary repeat diagnostic tests. For example, if a primary care provider already has the results of a recent MRI, the neurologist can access this information as well, saving time and resources.
- Integrated support systems: Continuous care involves integrating support systems such as social workers and occupational therapists who can provide additional resources and support to patients and their families, helping them navigate the complexities of brain health management.
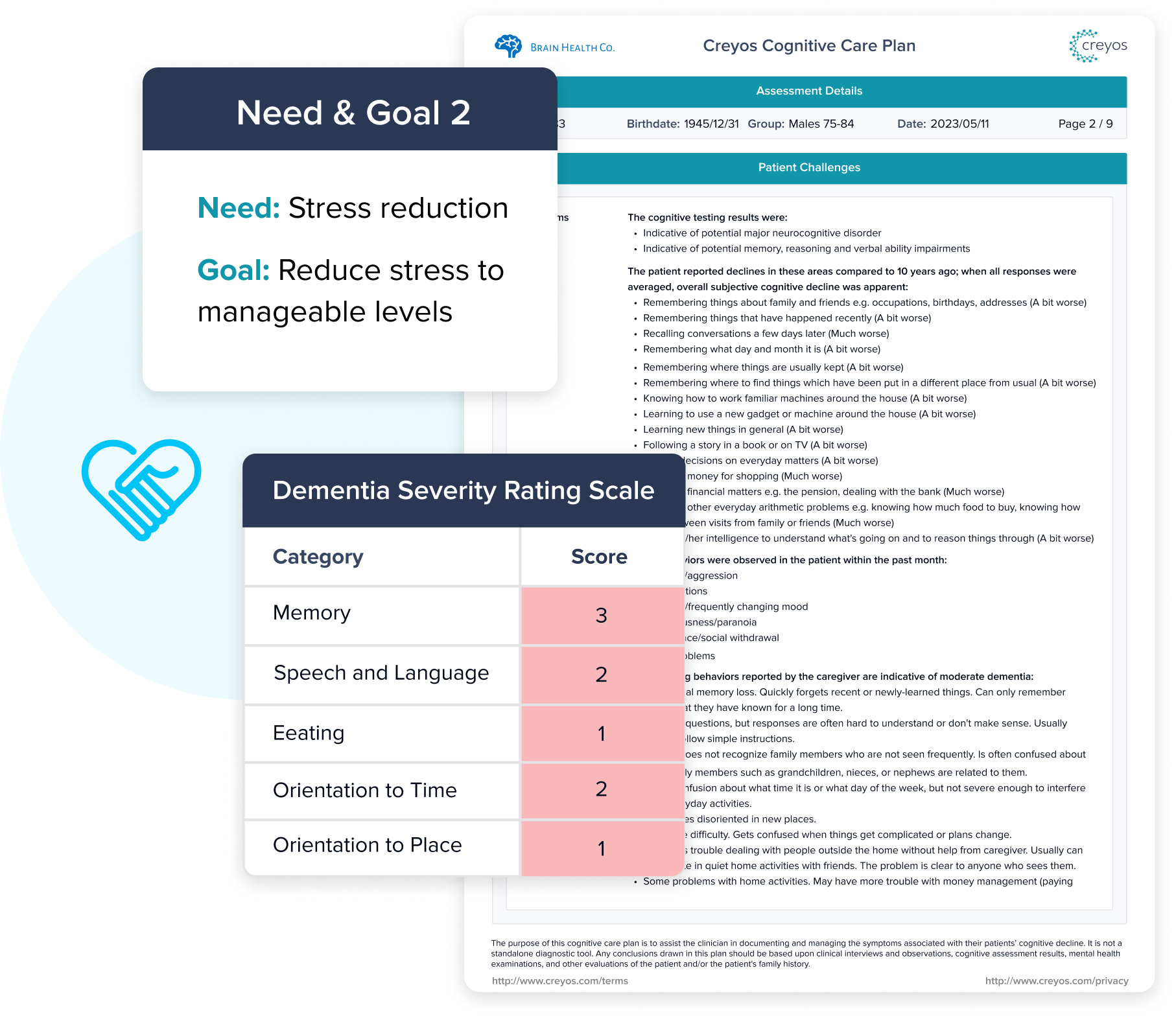
Create a Cognitive Care Plan
Creyos Health was designed specifically to deliver easy-to-interpret brain health reports, achieve seamless communication across providers, help retain patients and offer consistent care, and reduce administrative burden.
Learn more about measuring brain health and creating cognitive care plans on the platform.

Mental Health
Continuity of care in mental health services involves tight coordination between psychiatrists, psychologists, and primary care providers to ensure treatment plans remain consistent. It’s imperative that all therapeutic interventions and prescriptions are clearly communicated among various health providers. Those receiving care place high importance on readily available access to these services as well as support after leaving the hospital and from peers—elements deemed essential for sustained continuity (Psychiatric Services).
- Collaborative treatment plans: Mental health professionals work together to create comprehensive treatment plans. For example, a psychiatrist might coordinate with a psychologist to ensure that medication management and therapy sessions are aligned for a patient with depression.
- Clear communication of interventions: Ensuring that all therapeutic interventions and prescriptions are clearly communicated among various health providers helps avoid gaps or overlaps in treatment. For instance, a patient’s primary care provider should be aware of any psychiatric medications prescribed to avoid potential drug interactions.
- Continuous support systems: Access to continuous support systems, such as peer support groups or community mental health services, is crucial. For example, after hospital discharge, a patient might join a peer support group that provides ongoing emotional support and practical advice for managing their condition.
What is the Primary Goal of Continuity of Care?
At a high level, the objective of continuity in care is centered on advancing patients’ health by minimizing unnecessary handoffs between multiple providers—and improving information transfer and collaboration across the care team. Care continuity also encourages patient satisfaction and involvement through an approach where individuals feel attentively looked after.
Below, we’ll explore tactics and expected outcomes that ladder up to better care continuity.
Goals of Care Continuity
To enhance this aspect of healthcare delivery, strategies should include:
- Enhancing training and educational programs for providers
- Putting into place effective policies and governance frameworks
- Adopting approaches to care that prioritize the patient’s perspective
- Using technology to assist in creating seamless transitions
Focusing on these strategic areas can lead to streamlined processes, more integrated care provision, and robust relationships between patients and their healthcare providers—all fundamental components necessary in securing improved outcomes for patients as well as elevating the overall standard of healthcare quality.
Retaining Patients in Care
Maintaining patient engagement within the healthcare system (for as long as necessary) is fundamental to achieving successful outcomes. Several factors, especially those connected with continuity of care, might cause patients to disengage from their own healthcare journey:
- Inconsistent care providers: Frequent changes in healthcare providers can lead to a lack of trust and rapport.
- Poor communication: Ineffective communication between healthcare providers and patients can result in misunderstandings, lack of clarity about treatment plans, and unmet expectations.
- Complex healthcare systems: Navigating through a complex and fragmented healthcare system can be overwhelming for patients, leading to frustration and disengagement.
- Limited access to care: Difficulty accessing healthcare services, whether due to geographical barriers, long wait times, or financial constraints, can hinder patients' ability to stay engaged in their healthcare journey.
- Lack of personalized care: When care plans are not tailored to individual patient needs and preferences, patients may feel that their unique circumstances are not being considered.
- Insufficient follow-up: Lack of follow-up care or support after initial treatment can leave patients feeling abandoned and unmotivated.
- Technological barriers: Challenges in accessing or using healthcare technology can create barriers to engagement, especially for patients who are not tech-savvy.
Continuity of care best practices are designed to address and overcome the various challenges that can disrupt seamless healthcare delivery. Effective coordination, proactive management strategies, the integration of telemedicine, and virtual primary care help prevent discontinuities in care or unwarranted visits to emergency departments.
Reducing the Number of Touchpoints
How many touchpoints with a healthcare provider does a patient typically have? Medicare patients have reported receiving care from five or more physicians within the span of a year (Senate Committee of Finance). And for a single medical condition, some patients have as many as “50 interactions in a three-month period (through various modes of communication) between patient, primary care physician, and other physicians” (NEJM). Let’s expand on what this can look like:
Imagine a patient with dementia. They first visit their primary care physician, who refers them to a neurologist. At the neurologist's office, the patient must recount their entire medical history, including symptoms, previous cognitive function tests, treatments, and medications, despite having already provided this information to their primary care physician. After a few weeks, the patient is referred to a geriatric psychiatrist, where they once again have to repeat their medical history and treatment details.
This repetitive process frustrates the patient and makes them feel that the healthcare system is disjointed and inefficient. They feel like a number rather than a person, and their trust in healthcare providers diminishes. The lack of continuity in care means that each provider works with incomplete information, leading to miscommunication, redundant tests, and delays in receiving appropriate treatment. The overall experience is marred by unnecessary and redundant touchpoints, making the patient feel overwhelmed and undervalued.
Moreover, their caregiver, who often accompanies the patient to these appointments, experiences significant frustration as well. They must repeatedly explain the patient's condition and history to different providers, which can be emotionally exhausting and time-consuming. The caregiver's stress levels increase as they navigate the fragmented healthcare system, feeling as though they must constantly advocate for the patient to ensure they receive the necessary care.
By ensuring continuity of care through the use of electronic health records (EHRs) and coordinated communication among providers, these unnecessary touchpoints can be minimized. This would lead to a more streamlined and patient-centered experience, where the patient feels heard, respected, and efficiently cared for, and the caregiver experiences less stress and frustration.
Speeding up Time to Symptom Improvement
Continuity of care best practices are essential for speeding up the time to symptom improvement. By ensuring a unified and steady regimen, healthcare providers can create a seamless treatment experience that places the patient at the center. This approach fosters quicker relief from symptoms and improved overall health outcomes.
Research has shown that patients who experience continuous care are more likely to adhere to treatment plans and follow medical advice, leading to faster recovery times.
For example, one study (BMC Psychiatry) focused on the treatment of psychiatric disorders found that higher continuity of care significantly reduced symptom severity and significantly increased social functioning.
Another study (The British Journal of Psychiatry) looked at the long-term efficacy of a continuity-of-care treatment model for patients who transition from inpatient to outpatient services, resulting in significantly reduced admission time. In other words, patients were able to return to their everyday lives faster.
The results of this study underscored the effectiveness of a continuity-of-care model, which revolved around an integrated ‘continuity team’ led by senior psychiatrists and comprises paramedical personnel, including occupational therapists, psychologists, and expressive art therapists.
Symptom Relief in Fewer Visits
For another example of care continuity, read about how SohoMD stabilizes symptoms in as few as four appointments, using cognitive assessments that enable them to assess brain and mental health all in one platform.


Improved Patient Health Outcomes
Continuity of care is associated with improved health outcomes. Patients receiving consistent and cohesive medical services tend to follow through with medical recommendations, engage more in preventative healthcare measures, and have reduced instances of hospital admissions and emergencies.
Numerous studies have highlighted the positive impact of continuity of care on health outcomes. For example, a study published in BMC Psychiatry indicated that higher relational continuity of care for patients with serious mental illness may:
- Prevent premature deaths and suicide
- Lower the number of emergency department (ED) visits
- Contribute to a better quality of life compared to patients receiving lower levels of relational continuity of care
Implementing best practices such as interdisciplinary collaboration, effective communication, and personalized care plans ensures that patients receive consistent and cohesive treatment. This is particularly vital for individuals with complex health needs, as it allows for the integration of efforts across various healthcare providers, significantly accelerating the healing process.
Active patient engagement and involvement in their care journey further enhance the effectiveness of continuity of care. Patients who are well-informed and actively participate in their treatment plans are more likely to experience prompt symptom relief and better long-term health outcomes.
Improving Patient Satisfaction and Engagement
Improving both the satisfaction and active involvement of patients is at the heart of care continuity (JECP), which offers significant benefits such as:
- Strengthening the bond between patient and physician
- Promoting vigilant management of personal health
- Boosting patient adherence to recommended healthcare plans
- Empowering patients with knowledge to make well-informed decisions regarding their treatment
With digital engagement technologies (like cognitive testing) and resources enhancing continuity in healthcare, not only are health outcomes improved, but also the overall experience of receiving medical attention. This transforms recipients into engaged partners in managing their own healthcare paths.
What is a Continuity of Care Document?
A Continuity of Care Document (CCD) is a standardized electronic document designed to facilitate the exchange of patient information across different healthcare settings. The CCD is formatted in a standardized manner and contains critical aspects of an individual’s medical history, which allows for fluid exchange of information among various medical professionals.
This record ensures that every provider possesses the requisite knowledge to uphold the caliber and consistency of treatment provided, independent of their history with the patient or case. The primary goals of the CCD are to ensure continuity of care and improve patient outcomes by providing a comprehensive and up-to-date summary of a patient's health information.
Key Components of a CCD
A continuity of care document thoroughly details a wide range of information, covering:
- Patient information: Basic details such as the patient's name, gender, date of birth, and contact information.
- Healthcare provider information: Information about the patient's healthcare provider(s), including names, contact details, and roles.
- Medical history: A detailed record of the patient's history, including past illnesses, surgeries, hospitalizations, and treatments.
- Medications: A list of current and past medications, including dosages, frequency, and duration of use.
- Allergies and adverse reactions: Information about known allergies and any adverse reactions the patient has.
- Immunizations/vaccination history: A record of the patient's immunizations, including dates and types of vaccines received.
- Diagnostic test results: Results of recent diagnostic tests and procedures, such as lab tests, imaging studies, and biopsies.
- Care plan: The patient's care plan, including goals, planned interventions, and expected outcomes.
- Encounter information: Details of recent healthcare encounters, such as visits to healthcare providers, hospital stays, and emergency room visits.
- Functional status: Information on the patient's functional abilities, including mobility, self-care, and cognitive function.
- Advanced directives: Information about the patient's preferences for end-of-life care and advanced directives, such as living wills and durable power of attorney for healthcare.
The CCD incorporates detailed care plans that reflect the entirety of a patient’s health journey, helping to ensure that:
- Any new healthcare providers can swiftly gain insights into the individual’s medical attention
- The continuum of care is maintained with consistent information and communication within clinical settings
- There’s seamless interaction between electronic health records (EHRs)
The CCD also helps mitigate some of the common challenges to providing continuity of care, such as:
- A lack of availability from a patient’s regular health provider could break an existing therapeutic connection and diminish care continuity.
- The irregular presence of part-time providers potentially causes breaks in ongoing treatment.
- Shifts in health insurance may force changes among healthcare practitioners, thereby disrupting the smooth progression of care.
- Limitations on working hours within residency programs are other hurdles to continuous long-term engagement with patients. Although designed to safeguard residents’ well-being, these restrictions often lead to more frequent transitions between caregivers for patients and confusion about who holds responsibility for their treatment at any point.
These factors may complicate the evolving narrative of a patient’s medical experiences and pose difficulties in achieving steady provision of healthcare services but a CCD can help smooth those transitions.
Final Thoughts: Closing the Gaps In Care
Continuity of care is about connecting the dots in a patient’s healthcare journey, reducing complexities, and fostering a cohesive healthcare environment. By embracing the strategies and innovations discussed, healthcare providers can overcome challenges and improve patient outcomes.
 Reviewed by Mike Battista, Director of Science & Research at Creyos
Reviewed by Mike Battista, Director of Science & Research at Creyos
Mike Battista specializes in brain health, cognition, and neuropsychological testing. He received his PhD in personality and measurement psychology at Western University in 2010 and has been doing fun and useful stuff in the intersection between science and technology ever since.



