
Tools for Evidence-Based Practice in Cognitive Health Care
In today's changing medical landscape, cognitive health...
Read article
Published: 02/10/2025 | 8 min read
Written by: Louise Koren
Reviewed by: Mike Battista, Director of Science & Research, Creyos
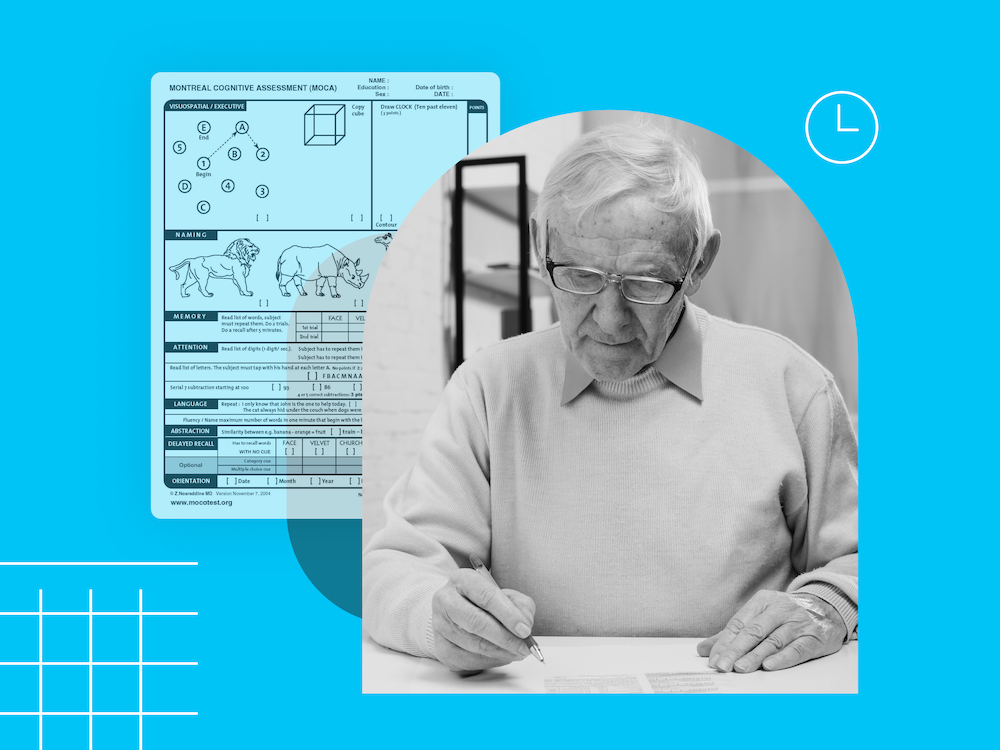
The Montreal Cognitive Assessment (MoCA) is a popular screening tool used to detect signs of cognitive impairment. But despite the popularity of the MoCA test among 63.8% of medical experts, up to 40% of primary care providers (PCPs) report that they don't feel confident making a dementia diagnosis. When it comes to dementia care, it’s early detection that creates the opportunity to improve patient outcomes.
Screening tools like the MoCA aren't detailed enough for PCPs to confidently diagnose dementia, and in-depth neuropsychological exams can take over a month to schedule. This gap in dementia detection shows there's a need for evidence-based assessments that are sensitive enough to catch earlier signs of Mild Cognitive Impairment (MCI), quicker to deliver accurate results to support diagnosis, and while there is still time to slow cognitive decline and plan for care.
In this article, we discuss the strengths and limitations of the MoCA test and how it compares to newer computerized cognitive assessment tools. We show how computerized testing procedures have the potential to fill the gap in detecting mild cognitive impairment, leading to more effective brain health treatments and better dementia care for patients.
The Montreal Cognitive Assessment is an eleven exercise cognitive test that takes approximately 10 minutes to complete. The MoCA was initially created in 2005 to improve upon the Mini-Mental State Examination (MMSE), which often fails to identify individuals with MCI.
Like all screening tests, the MoCA is considered a form of preventive care, as it is designed to detect mild cognitive impairment if conducted as part of a regular healthcare checkup. However, specialized testing via a neuropsychological exam is sometimes required to gather more detail or determine the source of a patient's cognitive difficulties—Alzheimer’s disease, Parkinson’s disease, vascular dementia, Lewy body dementia, or something else. Furthermore, the MoCA may have difficulty detecting milder declines in cognition before there is obvious subjective concern.
The MoCA test can be implemented as soon as a patient expresses that they're experiencing symptoms of cognitive dysfunction. If required, a primary care provider can then refer the patient to a neurologist for further testing. The neurologist might administer the MoCA as well, using it as a screener to test cognitive function before a neurological exam or other assessments. When cognitive deficits are confirmed and potential causes identified, a cognitive care plan can be created to enhance their quality of life, monitor treatment efficacy, detect changes to symptoms, and support their cognitive maintenance.
The patient's condition is assessed by calculating a total score across 11 exercises, with a maximum score of 30. According to the MoCA website’s guidelines, if a patient has a total score of 26 or higher, their cognitive health is considered normal, with normal cognition. Scores of 18 to 25 can indicate mild cognitive impairment, while scores of 10 to 17 can suggest moderate impairment. A score of less than 10 indicates severe impairment. Administering the MoCA and scoring a patient's answers requires certification training.
Once a primary care provider knows the MoCA's pros and cons, they can compare it with other assessments and make an informed decision on what's best for their practice and patients.
This guide explores how cognitive health technologies empower PCPs to deliver high-quality care efficiently, confidently, and at scale.
Creyos has a variety of cognitive solutions available to expedite the screening and diagnostic process, deliver accurate results, and support patient care and quality of life. Each tool is more detailed than traditional screening tools like the MoCA and quicker than full neuropsychological exams, while also being available through the convenience of an online, telemedicine-friendly platform.
The two-task cognitive screener is comparable to the MoCA, but takes less than three minutes to complete. The Creyos dementia screening test can detect subtle signs of cognitive impairment, and doesn't require training to administer or interpret. The screening results will indicate whether further testing is recommended to assist in the diagnosis of dementia or MCI.
If further testing is required, Creyos includes an assessment that provides detailed information about cognition in 20 minutes or less, which may assist with an accurate diagnosis. The assessment is a highly sensitive and scientifically validated six-task protocol. Once complete, it generates an easy-to-interpret report based on DSM-5 criteria for mild and major neurocognitive disorders. This allows healthcare professionals to quickly gain much of the information comparable to a neuropsychological exam, informing diagnosis, monitoring, and treatment plans.
Once a diagnosis is reached, Creyos comes with a built-in cognitive care plan. The care plan is based on guidelines by the Alzheimer's Association, and allows PCPs to provide support for caregivers and enhance patient quality of life. After a care plan is in place, cognitive assessment can be repeated to track treatment effectiveness and monitor patient symptoms over time, so PCPs can collect longitudinal data and make objective clinical decisions about next steps.

While the MoCA can be a useful tool to screen for cognitive impairment in patients, it takes more work on a PCP’s part to use it effectively and accurately.
To do so, healthcare professionals need to:
And even if a PCP follows these steps, there's always a chance that the results of the MoCA may be inaccurate due to factors like education or early symptoms that go undetected.
While the MoCA is used in many practices offering cognitive screening, healthcare professionals may want to consider additional options, like the Creyos cognitive assessments. These computerized neuropsychological assessments offer additional insights that aren’t offered by the MoCA and MMSE, while also being patient-friendly and efficient for clinicians. With the need for fewer referrals, this can free up providers’ time and lead to greater patient retention.
In one study comparing the MoCA and Creyos tests, borderline patients—those close to the MoCA cutoff—could be more confidently classified as impaired or unimpaired using a short set of Creyos tasks.
The Creyos assessments bridge the gap between an initial screening test (like the MoCA) and a neuropsychological exam, allowing providers to easily incorporate them into a more thorough testing process and improve dementia care. Additionally, the results are easy to interpret, don't require special training, and are instantly tabulated and compared to a diverse 85,000+ person normative database for demographic-specific results and pinpoint precision.
The Creyos Health platform is flexible enough to assess cognitive function in a wide variety of patients and use cases. Unlike the MoCA, the 20-minute Creyos assessment can be used to gain detailed information about multiple cognitive domains, compare the patient to age-matched norms, and includes mental health questionnaires, allowing PCPs to consider a patient's mental health conditions when assessing cognitive deficits.
Compared to traditional cognitive tests like the MoCA or MMSE, the computerized cognitive testing at Creyos is able to provide healthcare professionals with more detailed insight into a patient's cognition, while giving them the benefit of being tested at their own convenience.
While the MoCA is an accurate test when used as an initial screening tool for existing mild cognitive impairment, its disadvantages make it less appropriate as a diagnostic aid for MCI and dementia.
Instead of relying solely on the MoCA, consider bridging the dementia detection gap with highly sensitive computerized assessments. With digitized testing, primary care providers can increase the chances for early detection of MCI and dementia, expedite diagnosis, and enhance their patients' quality of life by getting them the right care before the disease progresses.
It is possible that a patient can pass the MoCA test and still have mild cognitive impairment or dementia. The MoCA is only one tool used to assess cognitive function, and its sensitivity is not perfect. With its short length, simple exercises, and other limitations, it cannot always pick up on every subtle sign of cognitive decline.
The opposite is also common: Patients who are cognitively healthy—as verified by detailed neuropsychological testing—can still score below 26 on the MoCA. These false positives, though unavoidable in any cognitive assessment, can cause unnecessary uncertainty while waiting for more detailed testing to confirm or rule out genuine cognitive deficits.
For healthcare professionals administering the MoCA test, including it within a broad range of assessments and ongoing cognitive health discussions is necessary to increase its effectiveness. A standalone test may not be enough to make a firm decision about a patient's condition.Unlike some other cognitive assessments, the MoCA requires the healthcare provider to complete a training and certification module. Only certified professionals have the training to interpret a patient's answers and assign appropriate scores to them. The downside is that this reduces the accessibility of the test, as not all PCPs or staff have the time or inclination to complete the training.
Traditionally, the MoCA has always been administered on pen and paper, but there are now versions available that can be accessed as a telehealth solution via the MoCA website or app.
 Reviewed by Mike Battista, Director of Science & Research at Creyos
Reviewed by Mike Battista, Director of Science & Research at Creyos
Mike Battista specializes in brain health, cognition, and neuropsychological testing. He received his PhD in personality and measurement psychology at Western University in 2010 and has been doing fun and useful stuff in the intersection between science and technology ever since.

In today's changing medical landscape, cognitive health...
Read article

Measurement-based care (MBC) gives healthcare providers the...
Read article

According to the World Health Organization (WHO), 22% of...
Read article