Creating a Care Plan: How to Help Someone With Cognitive Impairment
Published: 25/04/2024 | 9 min read
Written by: Lawrence Stewen
Reviewed by: Sydni Paleczny, Staff Scientist
Cognitive decline is on the rise as the aging U.S. population continues to grow, highlighting the importance of utilizing a cognitive test for dementia to identify early signs. But even though there's an increasing demand for cognitive care, only 50% of primary healthcare providers feel prepared to handle the needs of dementia patients.
This gap in cognitive care highlights the need for more sensitive screening tools that can detect mild cognitive impairment (MCI) and dementia in its earlier stages, when intervention may be more effective. These cognitive assessment tools also give primary care providers more time and resources to provide crucial education for patients faced with cognitive decline. One of those key pieces of education is a cognitive care plan.
In this article, we explain how to create a comprehensive care plan for patients with cognitive disorders, based on guidelines from the Alzheimer’s Association. Learn how to create a cognitive care plan and how computerized tests can help physicians meet rising demand while improving workflows and patient experience along the way.
When to Create a Cognitive Care Plan
Primary care physicians (PCPs) are often on the front lines of cognitive care, and increasingly dealing with an older population of patients. A cognitive care plan is best suited for patients with cognitive disorders, whether they’re older adults (65+ years old) or experiencing signs of earlier onset cognitive decline.
Patients with cognitive disorders include people with all kinds of dementia (including Alzheimer's disease), Parkinson's disease, traumatic brain injury, and other forms of cognitive decline. Studies indicate that 10% of adults 65 and up have dementia and 22% have MCI.
Care planning may also take place when a patient raises concerns about:
- Difficulty concentrating
- Memory impairment or problems
- Challenges with problem solving
- Spatial awareness and navigation problems
- Struggling to make simple decisions
- Difficulty following a conversation
The process of creating a care plan begins with cognitive testing to identify signs of impairment or decline. If a patient shows signs of a cognitive disorder or displays symptoms of one, a healthcare provider can raise the option for creating a care plan during an annual wellness visit, for example.
Combining Cognitive Screening with Care Planning
Cognitive assessment tools or screening tests are a key tool for care planning. A cognitive screen can be used to detect, monitor, and manage a patient’s MCI symptoms, while helping healthcare providers gather longitudinal data as their condition progresses.
As part of care planning, a healthcare provider might choose to schedule frequent reassessment to monitor the progression of a patient’s cognitive decline during their appointments.
For patients who are already diagnosed with a cognitive disorder, a care plan can help them achieve the best quality of life possible. With the support of their caregiver, a care plan can include steps to reduce symptoms or slow the disease's progression. Additionally, it can be used to plan end-of-life and palliative care procedures while the patient still has autonomy.
Using tools that provide objective cognitive performance data is one way to elevate patient care. Read more in our ebook: Connecting Care and Cognition.
How to Create a Care Plan for Cognitive Impairment
A primary care physician might initiate the process of care planning during an annual wellness visit, routine cognitive assessment, or another type of appointment. We’ve broken down the steps for creating a care plan into a few general steps to help guide the process.
Creating a care plan includes (but is not limited to) the following steps:
-
Assess patient cognition and symptoms
-
Evaluate caregiver needs
-
Build the care plan report
Below, we’ll outline each of these steps in more detail, including how to build a cognitive care plan in Creyos.
Assess Patient Cognition, Behavioral, and Neuropsychiatric Symptoms
A cognitive assessment for mild cognitive impairment equips healthcare providers with data to determine the severity of a patient’s disorder, map out its symptoms, and identify any mental health comorbidities.
Examples of assessments used in this process can include:
-
Mild Cognitive Impairment Screener or Assessment
-
BEHAV5+
-
IQCODE for subjective decline
-
IADL for functional independence
By capturing a baseline of a patient’s cognitive function, healthcare providers can reassess regularly and track any significant changes to cognition and mental health. These reports are useful in communicating with patients and caregivers, tailoring treatment, providing appropriate resources for the patient’s stage of cognitive decline, and monitoring symptoms over the course of the care plan.
Evaluate Caregiver Capabilities and Needs
Our recommendations here are based on examples of nursing assessments designed to evaluate a caregiver’s level of skill and expertise when supporting a patient with cognitive decline.
Evaluating the caregiver is also an opportunity to address their physical or mental health challenges, aspects of daily living, and potential caregiver stress. Then, a healthcare provider can recommend resources for preventing caregiver burnout and accessing community services that enable the caregiver to better support the patient.
Caregivers should be involved in the process of creating a cognitive care plan in order to:
-
Capture their insights about the patient’s independence and cognition
-
Communicate information that a patient might not be able to remember themselves
-
Equip caregivers to address patient’s needs outside visits with healthcare provider
-
Evaluate the caregiver’s skill and expertise
-
Assess the caregiver’s mental health and mitigate caregiver burnout
-
Provide social support groups and resources
Caregivers have a crucial role to play in conversations about a patient's cognitive condition. A cognitive care plan is built with sections specifically for caregivers—including discussing the results of an Instrumental Activities of Daily Living Scale (IADL) to help caregivers gain a better understanding of the patient's self care capabilities.
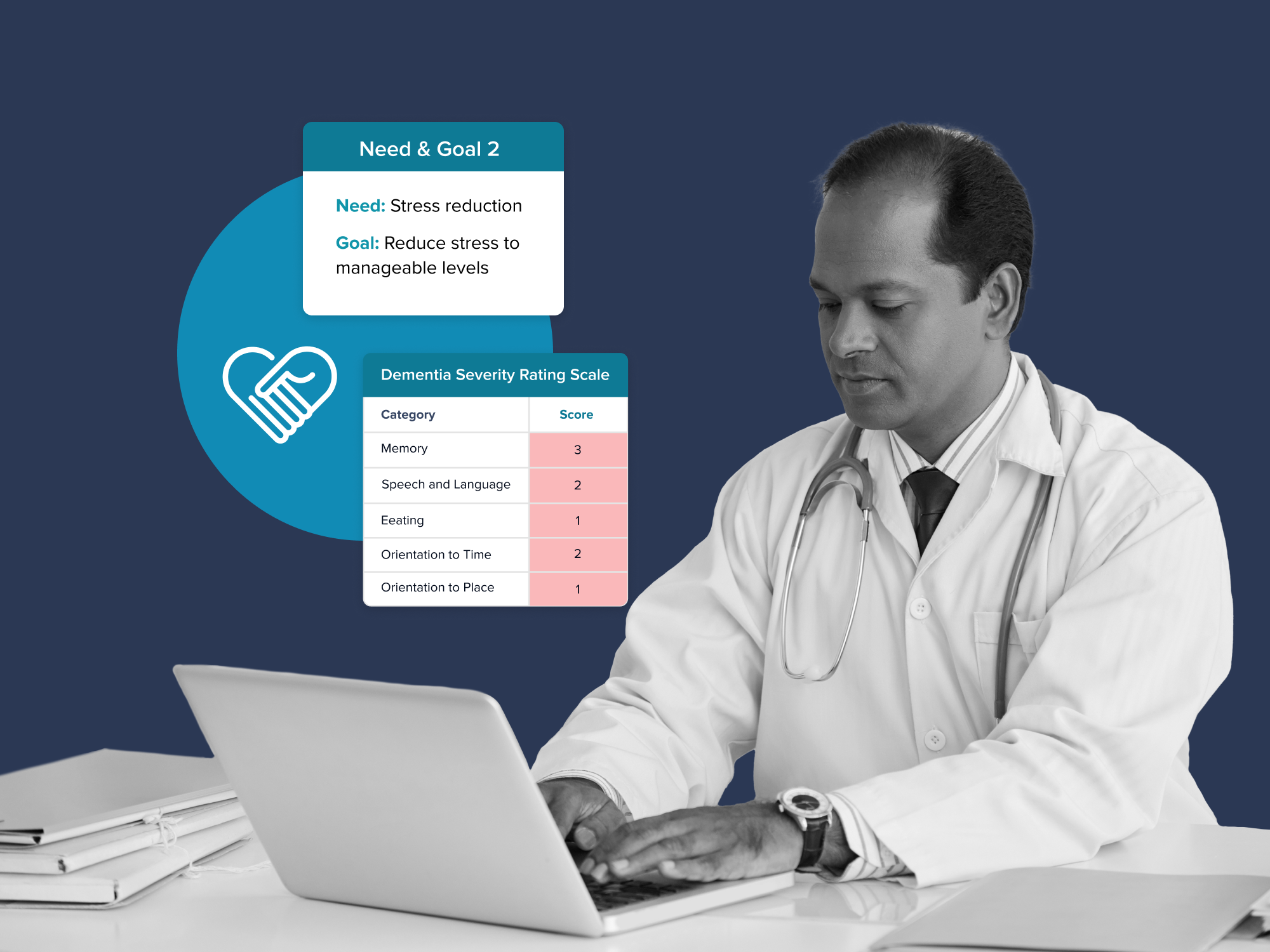
Another example is administering and discussing results from a Dementia Severity Rating Scale (DSRS), so that caregivers can better adapt their care for a dementia patient's needs. If the patient has severe dementia and is in the latter stages of decline, a caregiver should be involved in walking through an End-of-Life Checklist discussion.
Create a Care Plan
Building off of the cognitive assessment, the next steps of a care plan involve additional information gathering and putting together the plan. This means reviewing their medication on a regular basis, monitoring their symptoms, and assessing their safety and decision-making abilities as they go about their life.
A care plan is typically created during an in-person appointment, as communication and interpreting of cognitive assessment results with patients and caregivers are a requirement of effective care and necessary for reimbursement.
That said, the workflow involved with administering mental health questionnaires, cognitive re-assessment, and some elements of reviewing a care plan with patients can be streamlined using computerized cognitive assessments. Questionnaires and computerized cognitive assessments, for example, can be administered at home and the results can be reviewed in person.
A care plan can be read over by a caregiver under the supervision of a technician, and then further discussed with the primary care provider. A care plan might also involve multiple visits, particularly for patients with complex needs.
Read More: How to Bill Using CPT Code 99483 for Cognitive Care Planning
The Creyos Health platform can be used to create a care plan for cognitive impairment. It utilizes fully computerized assessments and data tracking all on one platform to maximize convenience for the patient and the clinic.
Here's how to create a cognitive care plan with Creyos:
- Log in to Creyos Health
- Create a new patient profile or click View Details on an existing record.
- On the Patient Details page, click Create Care Plan.
- If the patient has not yet completed the Dementia protocol, click Start Dementia protocol to administer it on the device you are using, or administer the protocol remotely by exiting the modal, clicking Start protocol, choosing the administration method, and then clicking Choose A Condition-Focused Protocol.
- If the patient has already completed the protocol, then simply click Create Care Plan.
- Follow the instructions carefully, and once you are done with the process, log back in to Creyos Health.
- Go back to the Patient Details page and click the Care Plans tab to review the full report summarizing the results of previous steps. You can also resume the care plan session from this section if the session ended prematurely.
- After reviewing the report with the patient and their caregiver, update the completion checklist and assign a follow-up appointment date. Click Save and then reopen the report to check that all of the patient's information has been captured before uploading it as an electronic medical record (EMR). This last step is mandatory in order to meet billing requirements.
Tips for Communicating With a Patient Who Has Cognitive Impairment
Communicating with patients who have cognitive and memory impairments can be difficult. They might struggle with keeping track of the conversation and may even misunderstand instructions about their care. Despite these challenges, knowing how to talk about cognitive health with them is a vital part of patient education.
Education that's clearly communicated can affect how a patient follows through with a healthcare provider’s recommendations. In fact, a systematic review found that 40% of studies reported improved health outcomes following educational intervention through an online portal. This suggests that educating patients, whether through online resources or clinical appointments, can directly affect the quality of their care.
Tips for healthcare providers:
-
Use simple, direct language. Present one new idea at a time, and try to ask yes-or-no questions or questions with multiple-choice answers.
-
Provide the patient with context. Explain what they should expect during their appointment.
-
Be aware that the patient may have audio, visual, or written communication difficulties. This may be exacerbated by existing health problems, such as poor vision, hearing, or chronic pain.
-
Make time to clarify answers and repeat questions. Help the patient understand the recommended treatment strategies and care management plan. Patient education has a significant impact on compliance and patient outcomes.
-
Schedule reassessment or follow up. Conclude the appointment by asking both the patient and caregiver to schedule an assessment or follow-up appointment.
What to Discuss With Patients and Caregivers
Now that we’ve reviewed why clear communication is important, it's time to dive into the content of those conversations. Many of these topics are built directly into care planning and cognitive assessment tools.
Here's a list of topics to guide cognitive care plan conversations with patients:
-
Diagnosis and Treatment Plan: Go over the diagnosis of their condition and explain their treatment plan. Ideally, this should happen at the early stages of their care plan, so they can take advantage of the benefits of preventive care.
-
Mental Health Comorbidities: It's possible that the patient may have a mental illness that's comorbid with their cognitive decline, such as depression. Educate the patient on how the two conditions affect each other, and what they can do to minimize the effects.
-
Medication Management: If the patient requires medication, or if they are taking medication for separate conditions, it's vital to schedule a medication review to discuss potential side-effects and drug interactions.
-
Safety Concerns: Highlight any risks that may result from the treatment plan or aspects of the patient's life—such as their living situation.
-
Aids for Daily Functioning: Suggest simple solutions that can make the patient and caregiver's daily life easier. For example, dementia patients tend to prefer a daily routine and an organized home with clear labels to show where items are located.
-
Healthy Lifestyle Recommendations: Staying in good physical health via exercise, a nutritious diet, socialization, mental stimulation, and so on are all modifiable risk factors that can prevent dementia or slow down its progress.
-
Identify Additional Family Member Caregivers: To prevent caregiver burnout, identify additional family members who may be willing to contribute or step-in when the primary caregiver is occupied.
-
Social Supports and Services: Even in the care where there are other family caregivers available, provide the caregiver with ways to contact social support services for respite care and financial aid.
-
Caregiver Support Resources: If the caregiver is feeling isolated and stressed due to their role, a healthcare provider may want to suggest community resources, support groups, or other local resources. Caregiver role strain is a serious condition, but there are many resources available to minimize its effects and find emotional support.
By raising these topics to the patient and their caregiver, healthcare providers can proactively prepare them for their roles. Every health journey is a partnership, and the more patients and caregivers learn about how to manage symptoms and reduce stress, the better their well-being.
Why Use Computerized Tests and Cognitive Care Planning
While a cognitive care plan can be administered through traditional pen and paper assessments and in-person clinic appointments, a patient will be missing out on the more convenient care opportunities that come from a digitized care plan.
Computerized tests allow a patient to take assessments from the comfort of their own home and at their own convenience. They won't have to stress out about missing an appointment, or worry about traffic along the way. A digital platform gives healthcare providers the opportunity to schedule concise assessments and check-ins in closer succession, keeping patient data as objective and accurate as possible.
The Creyos Cognitive Care Plan is informed by the Alzheimer's Association, but presented in a way that's much faster to administer and more convenient for patients, caregivers, and clinicians.
Here's what to expect:
- Administer assessments in parts, or allow the patient to take home a comprehensive assessment package.
- Have a technician oversee elements of the digital screening and questionnaire process, such as report interpretation, so that physicians can have a more focused use of in-person appointment time with the patient.
- An all-in-one platform that allows for longitudinal cognitive tests, mental health questionnaires, cognitive tests for dementia, and independent living evaluations like the Instrumental Activities of Daily Living Questionnaire(IADL).
- The ability to integrate patient records with a selection of other platforms and systems.
- Organized documentation and note taking tools.
- Built-in resources to support patient care and caregiver groups and services.
- Automated scheduling and email integration built into the platform.
- Designed with reimbursement guidelines in mind, helping a practice increase its revenue by meeting CPT code 99483 requirements.
All of these activities are integrated into one seamless platform and workflow. The results of cognitive and mental health assessments, and care planning, are collected into one PDF report automatically and instantly. These automations can save physicians from juggling separate printed reports. The integrated platform is also a significant time saver, as session notes are automatically uploaded to patient records.
Improving the Cognitive Care Planning Process
Knowing how to help someone with cognitive impairment is not simple, but the process can get easier with a solution that's customized to suit their needs. A computerized cognitive care plan can help healthcare providers improve the health care of their patients, while also making workflows more time- and cost-efficient. As the U.S. population ages and health professionals see more patients with cognitive disorders on their appointment lists, cognitive care planning may be instrumental in improving patient quality of life while also preparing healthcare practices for the future.

Reviewed by Sydni Paleczny, Staff Scientist
Sydni earned her MSc in Neurosciences at Western University under Dr. Adrian Owen. Her research explores neuropsychological outcomes after cardiac surgery, with interests in cognitive neuroscience, critical care, and brain health. At Creyos, she supports scientific validity, health technology, and ongoing research.


