
The Profound Interplay Between Sleep and Cognitive Function
Published: 14/08/2025 | 8 min read
Written by: Mackenzie Godard
Reviewed by: Mike Battista, Director of Science & Research
Sleep, far from being a passive state of rest, is a dynamic and essential process that profoundly impacts every facet of our cognitive performance and overall brain health. For healthcare providers, neuroscientists, neuropsychologists, and mental health professionals, understanding the intricate relationship between sleep and cognitive function is essential for comprehensive patient care (Ramar et al., 2021).
This article delves into the critical role of sleep in maintaining and optimizing cognitive abilities, exploring the consequences of sleep deprivation, and the way that healthy sleep habits support brain function, information processing, and long-term cognitive health.
The Foundation of Cognitive Performance: Why Sleep Matters
Sleep and cognitive function are inextricably linked (Khan et al., 2023). A person’s waking hours require strong cognitive performance, with daily lives requiring constant decision-making, problem-solving, attention, and concentration.
Without adequate sleep, these abilities may quickly diminish, leading to observable impairments in various cognitive processes (Wild et al., 2018). Even a single night of sleep loss can have measurable negative effects on the human brain (Krause et al., 2018).
Sleep research consistently shows that the brain remains highly active during sleep, engaging in vital processes for restoring mental faculties and consolidating information (Walker, 2024; Whitehurst et al., 2022). This suggests that sleep supports functions beyond physical rest; it optimizes the cognitive abilities that underpin our capacity to engage with the world.
The Stages of Sleep and Their Cognitive Roles
To fully appreciate the relationship between sleep and cognition, it’s essential to understand the different sleep stages and their unique contributions to brain function.
Sleep cycles through two primary states: non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. Each stage plays a distinct role in memory consolidation and other cognitive processes.
NREM Sleep: The Mastermind of Memory Consolidation
NREM sleep is further divided into multiple stages, with the deepest stage (N3, or slow wave sleep) being particularly crucial for memory consolidation. During slow-wave sleep, the brain exhibits characteristic slow oscillations and slow-wave activity.
These oscillations are thought to facilitate the transfer of newly acquired information from the hippocampus to the neocortex, where memories are stored longer-term. This process is vital for declarative memories, events, and concepts (Sridhar et al., 2023).
Studies using functional magnetic resonance imaging (fMRI) have found increased activity in specific brain regions during slow-wave sleep, correlating with the reactivation of learning experiences from the preceding day (Brodt et al., 2023). This memory replay mechanism can help to strengthen neural connections, embedding knowledge for long-term retention.
Beyond declarative memories, NREM sleep also supports the consolidation of procedural memory (the learning of skills and habits), like riding a bike or playing an instrument (Christova et al., 2018). The precise mechanisms differ, but the general principle is that NREM sleep is a prime time for the brain to solidify learning.
REM Sleep: Emotional Processing and Creative Insight
Between cycles of NREM sleep, we enter REM sleep. This stage is characterized by rapid eye movements, increased brain activity, and vivid dreaming.
While slow wave sleep is important for declarative memory, REM sleep is thought to be more involved in the consolidation of emotional memory and the integration of new information into existing knowledge networks, potentially fostering creativity and problem-solving (Lewis et al., 2018).
The interplay between NREM and REM sleep provides a balance between memory consolidation and cognitive restoration. Disturbances to this natural sleep-wake cycle can disrupt these processes, leading to significant cognitive impairment (Reddy et al., 2023).
The Harmful Effects of Sleep Deprivation
The impact of sleep loss on cognitive function is extensive and well-documented through decades of sleep research (Killgore, 2010; Waters et al., 2011). A sleep-deprived human brain often struggles with:
- Attention and vigilance: Sustaining focus becomes challenging, leading to increased errors and slower reaction times. This is particularly evident in tasks requiring sustained attention, like driving or operating machinery (Gottlieb et al., 2018).
- Working memory: The ability to hold and manipulate information in the short term (our working memory) may be less susceptible to the effects of sleep deprivation than other cognitive abilities. People with sleep deprivation or who get less sleep than normal generally do not show impairment in working memory tasks.
- Decision-making and problem-solving: Executive functions like planning, judgment, and impulse control can be significantly impacted by sleep deprivation. This can lead to risky decision-making and impaired problem-solving abilities (Salfi et al., 2020; Wild et al., 2018).
- Mood and emotional regulation: Poor sleep can exacerbate irritability, anxiety, and stress, making it difficult to regulate emotions (Vandekerckhove et al., 2017).
- Creativity: The flexible thinking often linked to creativity is hampered by a lack of sleep, particularly as REM sleep is disrupted (Landmann et al., 2015).
Even minor reductions in sleep duration can accumulate into a sleep debt and result in significant cognitive decline over time. This chronic insufficient sleep can manifest as persistent fatigue, reduced productivity, and an increased risk of accidents.
How Sleep Disorders Can Impact Cognitive Decline
For many, sleep loss may be a symptom of an underlying sleep disorder (Hanson & Huecker, 2023). Conditions like sleep apnea and insomnia can severely disrupt sleep patterns, leading to fragmented or otherwise poor sleep that prevents the brain from completing restorative processes.
Sleep apnea
Characterized by repeated interruptions in breathing during sleep, sleep apnea leads to fragmented sleep and reduced oxygen to the brain. This chronic disruption can be a serious contributor to cognitive impairment. Sleep apnea is also increasingly recognized as a risk factor for neurodegenerative conditions like Alzheimer's disease (Andrade et al., 2019).
Insomnia
The inability to fall or stay asleep can lead to chronic sleep restriction and pervasive cognitive decline. Individuals with insomnia often report difficulties with working memory and concentration (Brownlow et al., 2019).
Diagnosing and treating these sleep disorders is a critical step in preserving brain health and mitigating cognitive impairment. Healthcare providers should screen for sleep disturbances as part of a comprehensive assessment of a patient's cognitive health.
The Link Between Sleep, IQ, and Long-Term Cognitive Health
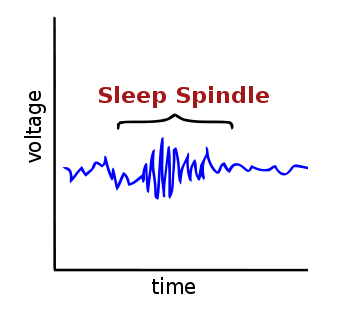
Sleep research has uncovered fascinating connections between specific sleep characteristics and measures of intelligence (Ujma et al., 2020). One notable area of study is that of the relationship between sleep spindles and IQ (Fang et al., 2017).
Sleep spindles, short neural oscillations that occur during NREM sleep, have been consistently linked to cognitive performance (Bódizs et al., 2014). Research suggests that rather than being a side effect of sleep quality, there is a deeper relationship between these specific patterns of brain activity during sleep and intellectual capacity. This finding emphasizes the intricate ways that the activity of the brain during sleep is linked with our cognitive abilities (Fang et al., 2017).
Looking beyond intellectual ability, the long-term impact of sleep on healthy cognitive aging is a growing area of focus for brain research. Chronically poor sleep is increasingly recognized as a risk factor for accelerated cognitive decline and neurodegenerative diseases (Ungvari et al., 2025).
Sleep fragmentation and reduced slow wave activity in middle age have been linked to an increased risk of developing Alzheimer's disease in later life. This is thought to be partly due to sleep's role in the clearance of amyloid-beta and tau proteins, which accumulate in the brains of Alzheimer's patients. Proper sleep can help the brain's glymphatic system flush out these metabolic waste products, preventing their buildup and potential neurotoxic effects (Reddy et al., 2020; Lucey et al., 2020).
Optimizing Sleep for Better Cognitive Performance
Given the compelling evidence for the importance of sleep, promoting healthy sleep habits is essential to maintaining and improving cognitive performance and overall brain health. Healthcare providers can support healthy sleep habits by educating patients on strategies to improve sleep quality, like:
- Establishing a regular sleep-wake cycle: Going to bed and waking up at consistent times, even on weekends, helps to regulate the body's natural circadian rhythm, making it easier to fall asleep and wake up refreshed (Windred et al., 2024).
- Creating a conducive sleep environment: A dark, quiet, and cool bedroom promotes better sleep (Dautovich et al., 2022). Minimizing exposure to bright screens (especially blue light) before bed can also significantly improve sleep quality (Ishizawa et al., 2021).
- Limiting stimulants and alcohol: Caffeine and nicotine intake, particularly in the afternoon and evening, can interfere with sleep. Alcohol, while initially seeming to induce sleepiness, often disrupts sleep stages later in the night, leading to fragmented rest (Colrain et al., 2018).
- Incorporating regular physical activity: Exercise can improve sleep quality, efficiency, and duration, but it's important to avoid intense workouts too close to bedtime (Dolezal et al., 2017; Leota et al., 2025).
- Managing stress: Chronic stress can interfere with sleep. Techniques like mindfulness, meditation, and other relaxation exercises can help calm the mind before bed (Rusch et al., 2018).
- Addressing sleep disorders: For patients experiencing chronic excessive sleepiness or difficulties sleeping, a thorough evaluation for sleep disorders like sleep apnea or insomnia is crucial. Treating these conditions can improve both sleep quality and cognitive function (D’Rosario et al., 2022).
The Evolution of Sleep Research and Cognitive Health
The field of sleep research continues to examine the complex ways in which sleep influences our minds. Advanced neuroimaging techniques, like new methods of gathering and interpreting MRI data, are providing insights into the brain regions and neural circuits active during different sleep stages and how they contribute to memory and other cognitive processes (Syväoja et al., 2025).
As we gain a deeper understanding of the molecular and cellular mechanisms underlying the cognitive benefits of sleep, we move closer to developing more targeted interventions for individuals struggling with sleep loss and cognitive impairment.
Moreover, as sleep is increasingly recognized as a pillar of health, sleep interventions are becoming an even more integral part of primary care and preventative health strategies. Professionals are more equipped to discuss sleep habits, assess sleep duration, and recommend interventions to help patients achieve restorative sleep for better cognitive performance.
Key Takeaways
Sleep is invaluable to cognitive health.
Research shows that sleep plays an invaluable role in maintaining optimal cognitive performance and preserving brain health. From supporting reasoning abilities and memory consolidation to protecting against cognitive decline and conditions like Alzheimer's disease, proper sleep is fundamental for a healthy mind.
Effective sleep assessments better support comprehensive patient care.
For healthcare providers, integrating comprehensive sleep assessments is valuable for supporting comprehensive patient care. In addition to cognitive assessment, Creyos Health offers scientifically backed standardized sleep questionnaires, like the PSQI, designed to assess patients’ sleep quality, patterns, and disturbances over time to help inform treatment interventions for sleep disorders.
There is an intricate relationship between sleep and cognitive function.
By understanding the intricate relationship between sleep and cognitive function, and addressing patients’ sleep deficits and disorders, providers can help them unlock their full cognitive potential and long-term brain health. In a world that often undervalues rest, championing the importance of adequate sleep is one of the most powerful contributions providers can make to patients' well-being.
Frequently asked questions
What are the cognitive effects of sleep deprivation?
What are the stages of sleep?
What can I suggest to patients to improve their Sleep for Better Cognitive Performance?
There are many different ways that individuals can improve their sleep quality and quantity. Some of the most common and effective recommendations are:
- Establishing a regular sleep-wake cycle
- Creating a conducive sleep environment
- Limiting stimulants and alcohol
- Incorporating regular physical activity
- Managing stress
- Addressing sleep disorders

Reviewed by Mike Battista, Director of Science & Research at Creyos
Mike Battista specializes in brain health, cognition, and neuropsychological testing. He received his PhD in personality and measurement psychology at Western University in 2010 and has been doing fun and useful stuff in the intersection between science and technology ever since.

