
Top Benefits of Telehealth Implementation in Cognitive Healthcare
Following the COVID-19 pandemic, telehealth implementation...
Read more



Uncertainty delays diagnosis, care planning, and proper risk adjustment, which limits effectiveness of clinicians.
Specialists are overwhelmed—referrals don’t happen fast enough and there can be a wait time of 3-6 months.
Traditional tools like the MMSE are limited and lack sensitivity for accurate, early screening.

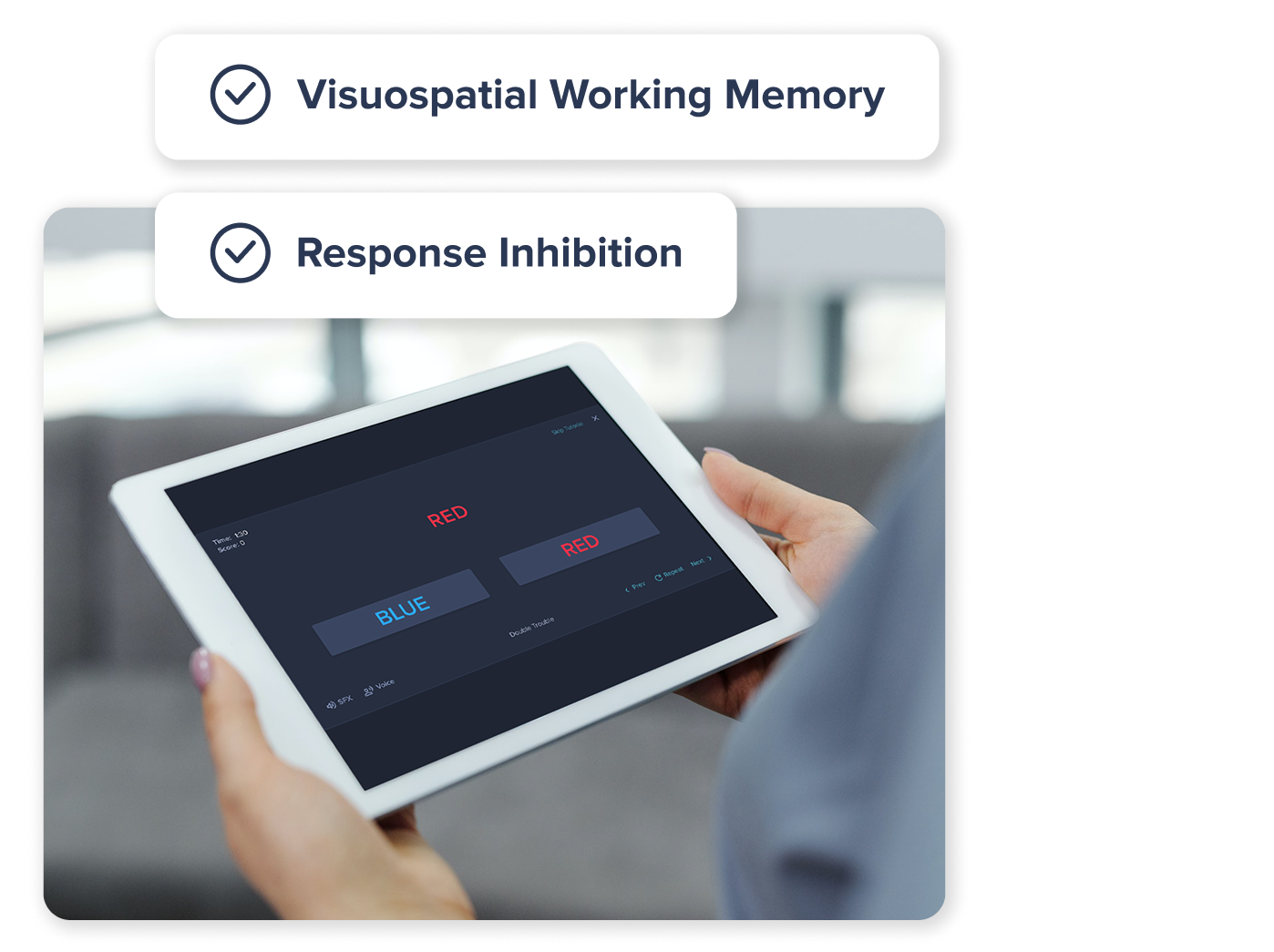
Fast and efficient—can be completed remotely without physician oversight
Inefficient and difficult to administer—require physician oversight
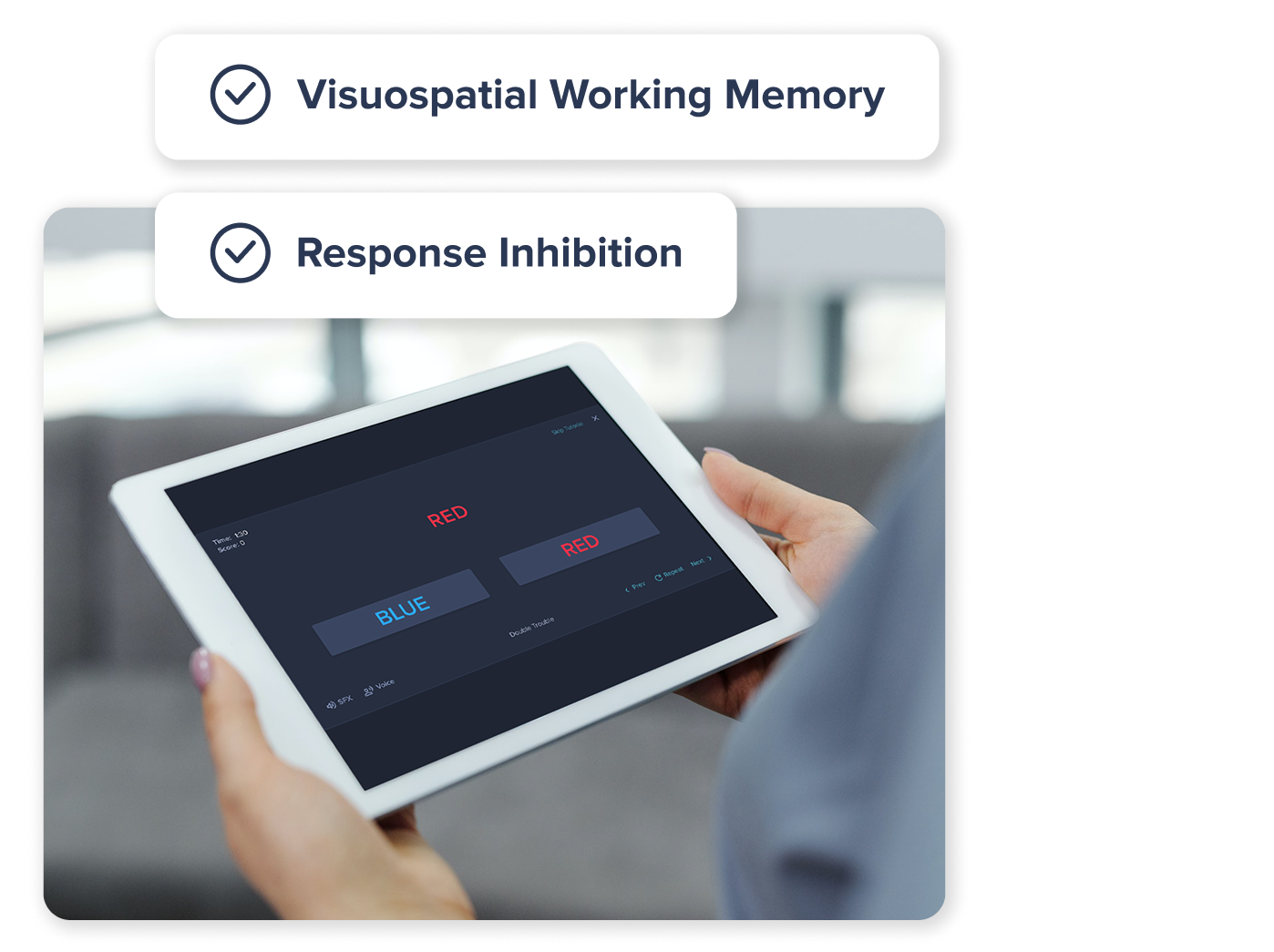
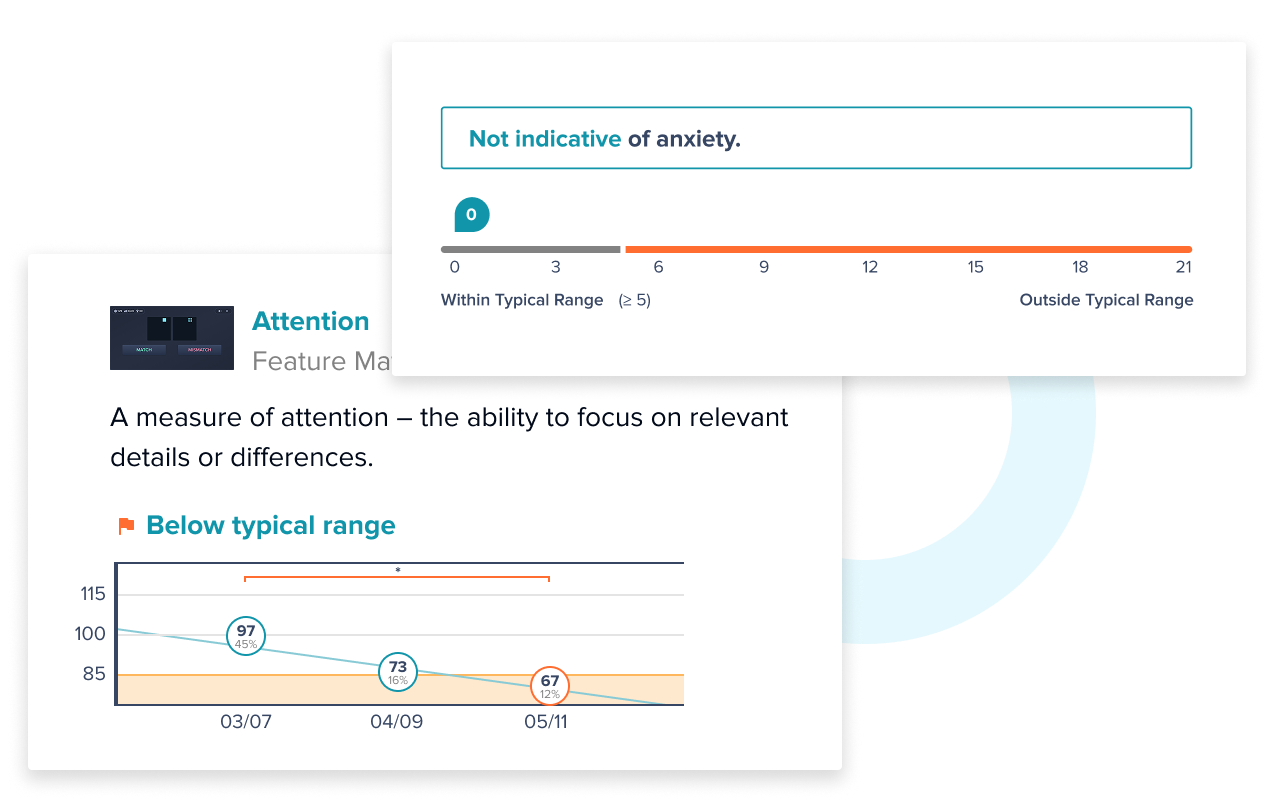
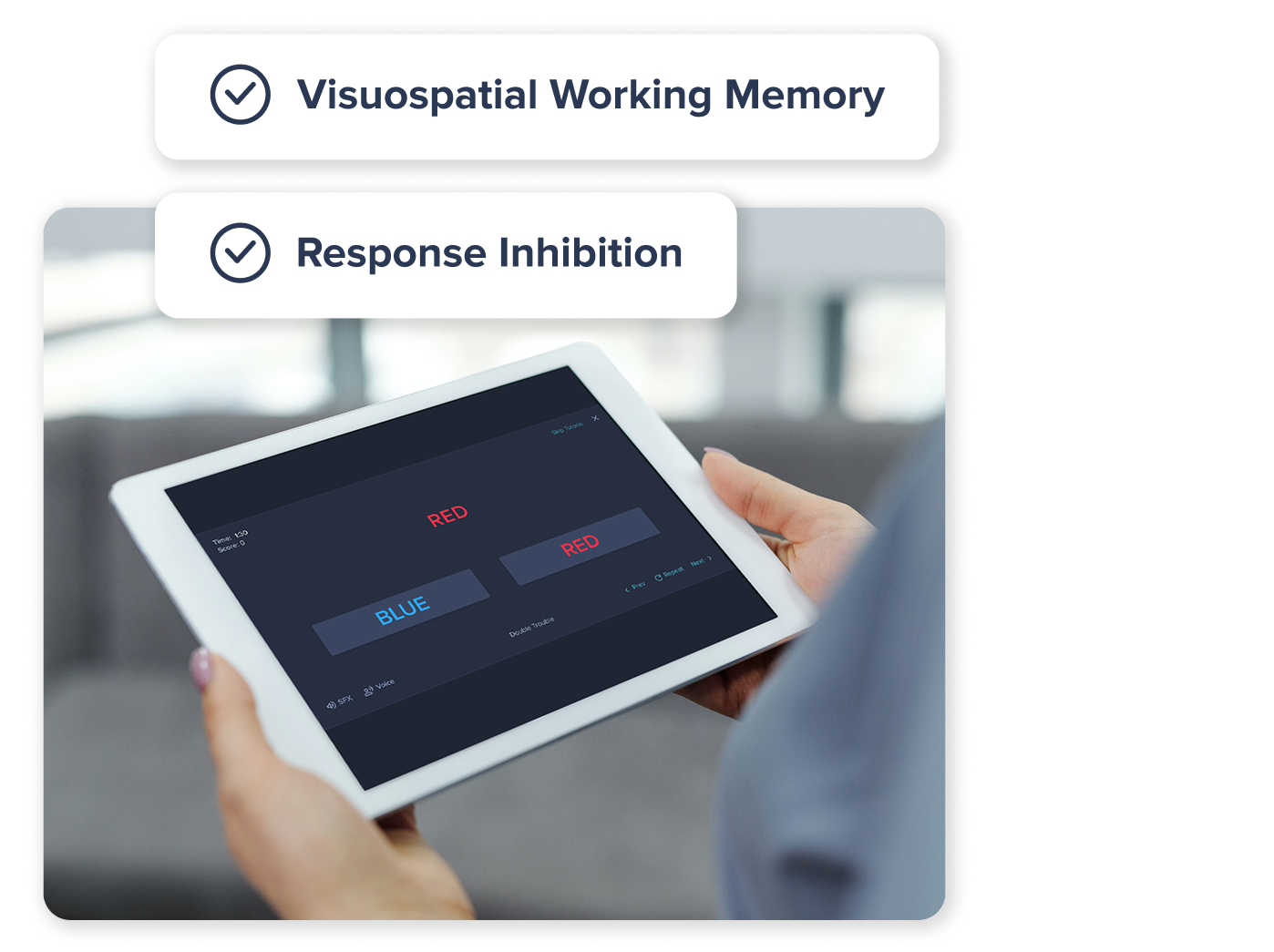
Designed for early detection of subtle changes in cognitive function
Designed specifically for individuals with potentially significant cognitive issues
Associated with distinct brain regions and functions, as validated by fMRI
No alignment to brain regions or specific cognitive domains
Sensitive to factors that can impact brain health, such as: lifestyle, mental health concerns, neurological conditions, etc.
Minimal utility for the general population with limited sensitivity to certain conditions and disorders (e.g., ADHD, depression, anxiety, etc.)
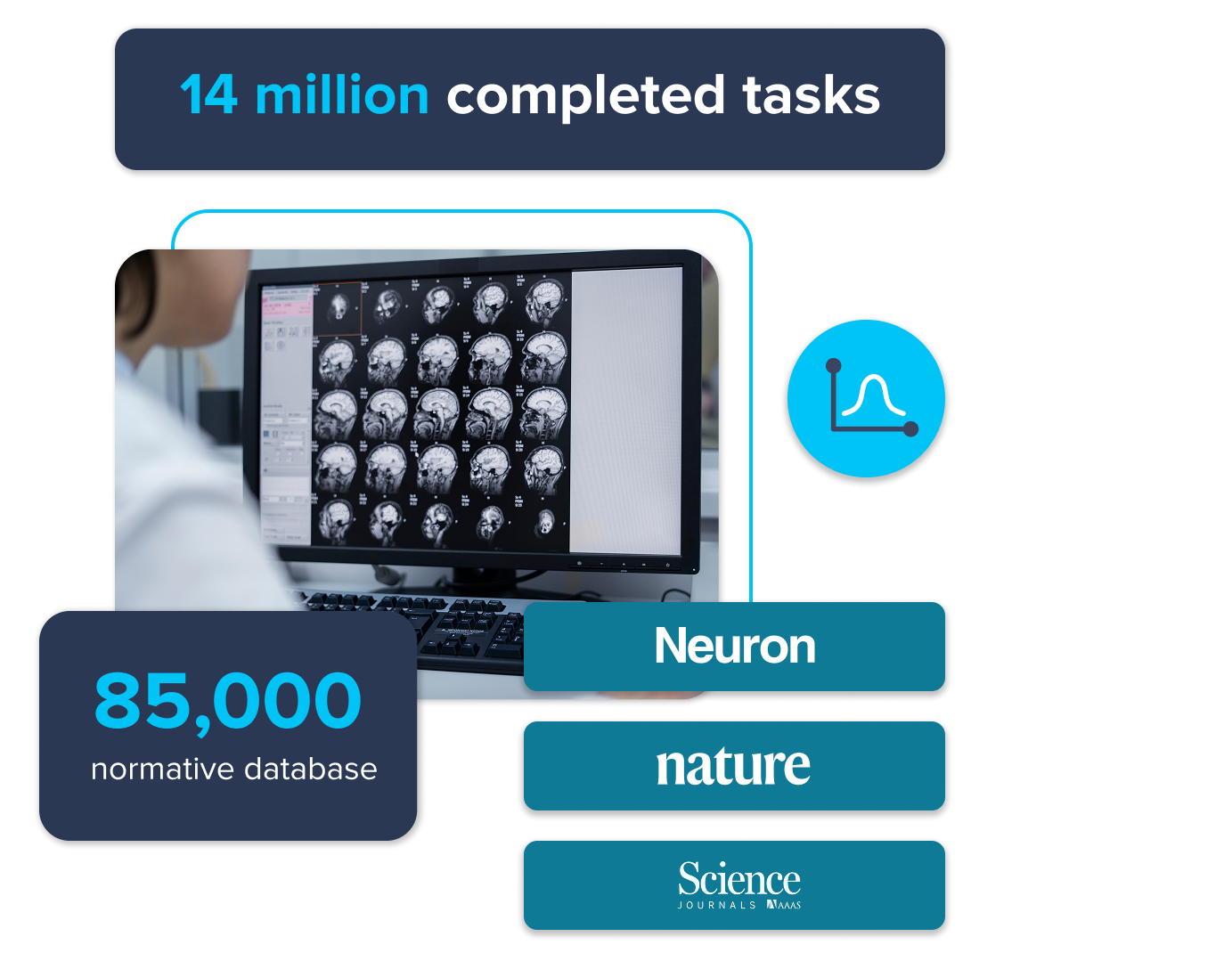
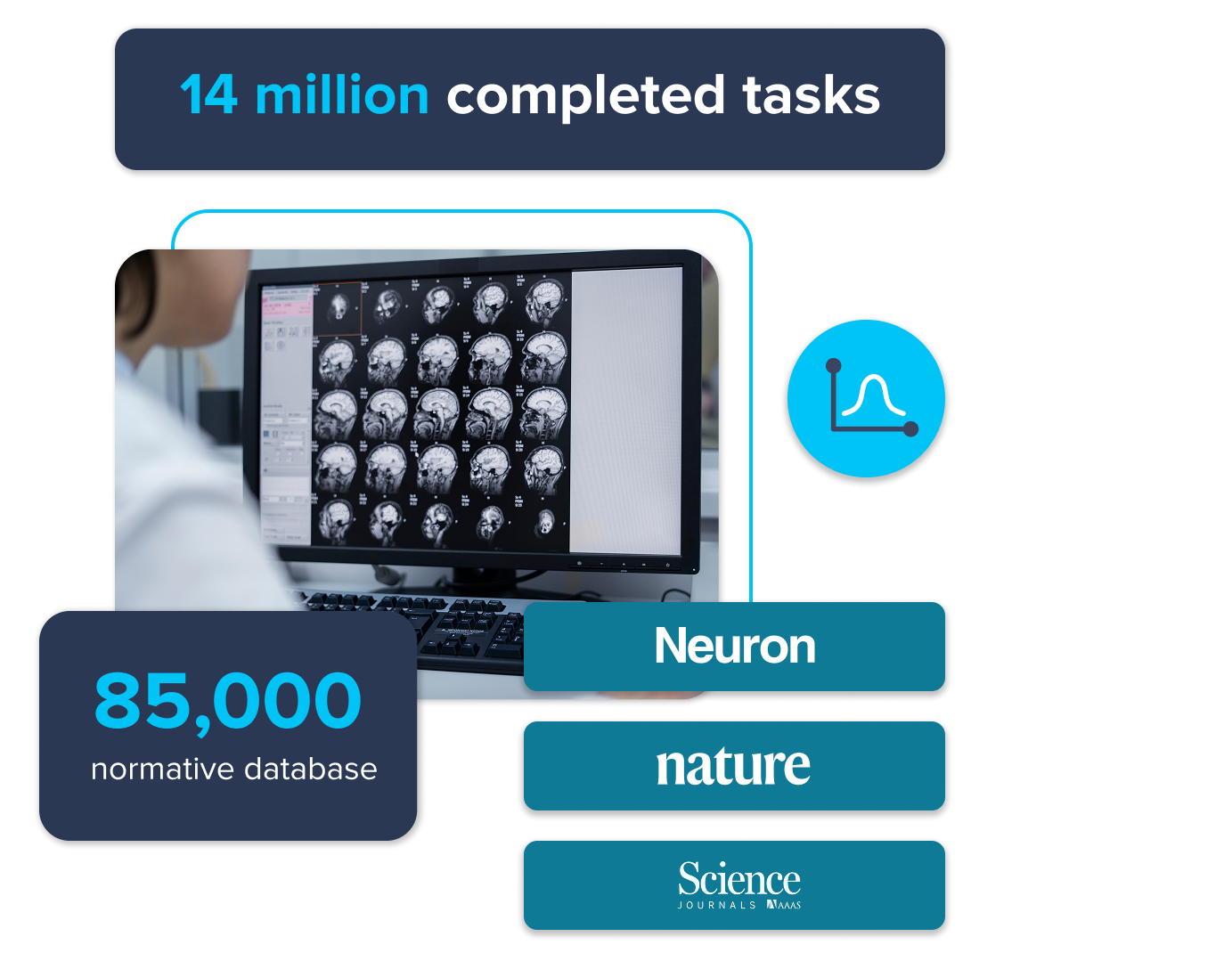
Utilizes 85,000+ participant normative databases to classify patients as below average, average or above average relative to their demographic group
Returns a single, non-specific number that provides little context or insight regarding areas of deficit
Excellent test-retest reliability—designed for longitudinal monitoring
Not well suited to longitudinal monitoring
Please note: The Creyos dementia protocol is not a standalone diagnostic tool. As with other Creyos Health assessments, any conclusions drawn from the Creyos dementia protocol should be paired with clinical interviews and observations, other mental health examinations or assessments administered, and other evaluations of the patient and/or the patient's family history
Specificity Concern: Studies have reported low specificity, increasing the risk of false positives. In one review, specificity was as low as 35% depending on the context, which may reduce diagnostic accuracy in certain patient populations.¹
Limited Sensitivity and Ceiling Effects: May miss early decline—one study found a 34% false negative rate using a cutoff of 24.² Its ceiling effect also makes it harder to distinguish normal aging from mild cognitive impairment (MCI).³
Variable Sensitivity and Specificity: Performance varies by setting. Though sensitive to dementia, one study showed only 54% specificity, potentially limiting its reliability as a standalone screening tool for conditions like dementia.⁴
1. Kansagara, D., & Freeman, M. (2010). A Systematic Evidence Review of the Signs and Symptoms of Dementia and Brief Cognitive Tests Available in VA. Department of Veterans Affairs (US). https://www.ncbi.nlm.nih.gov/books/NBK49027
2. O’Bryant, S.E., Humphreys, J.D., Smith, G.E., Ivnik, R. J., Graff-Radford, N. R., Petersen, R. C., & Lucas, J. A. (2008). Detecting Dementia With the Mini-Mental State Examination in Highly Educated Individuals. Arch Neurol, 65 (7), 963–967. https://doi.org/10.1001/archneur.65.7.963
3. Trzepacz, P. T., Hochstetler, H., Wang, S., Walker, B., & Saykin, A. J. (2015). Relationship between the Montreal Cognitive Assessment and Mini-Mental State Examination for assessment of mild cognitive impairment in older adults. BMC Geriatrics, 15 (107). https://doi.org/10.1186/s12877-015-0103-3
4. Kaufer, D. I., Williams, C. S., Braaten, A. J., Gill, K., Zimmerman, S., & Sloane, P. D. (2008). Cognitive Screening for Dementia and Mild Cognitive Impairment in Assisted Living: Comparison of 3 Tests. Journal of the American Medical Directors Association, 9(8), 586–593. https://doi.org/10.1016/j.jamda.2008.05.006


Fast, Digital Cognitive Testing
Clear Clinical Reports
Designed for Primary Care Workflows
Backed by Decades of Scientific Research

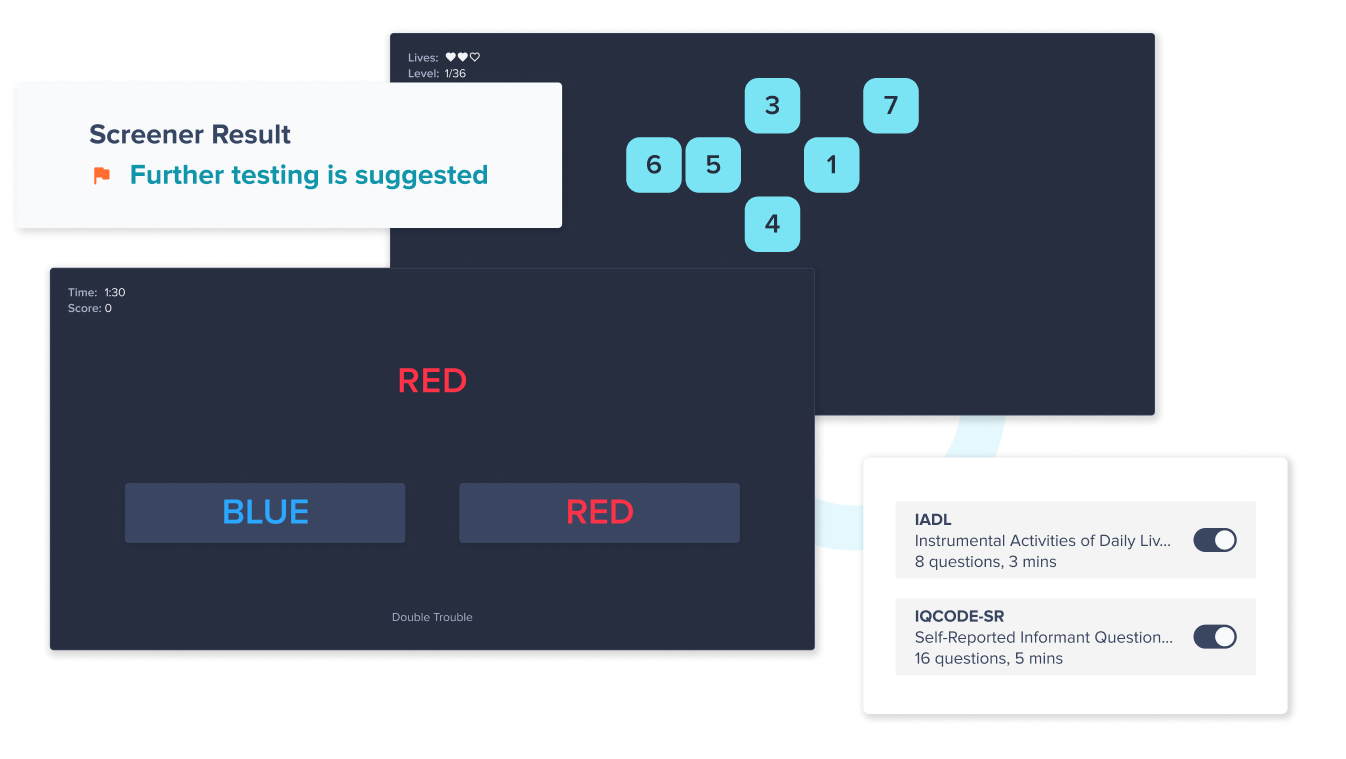
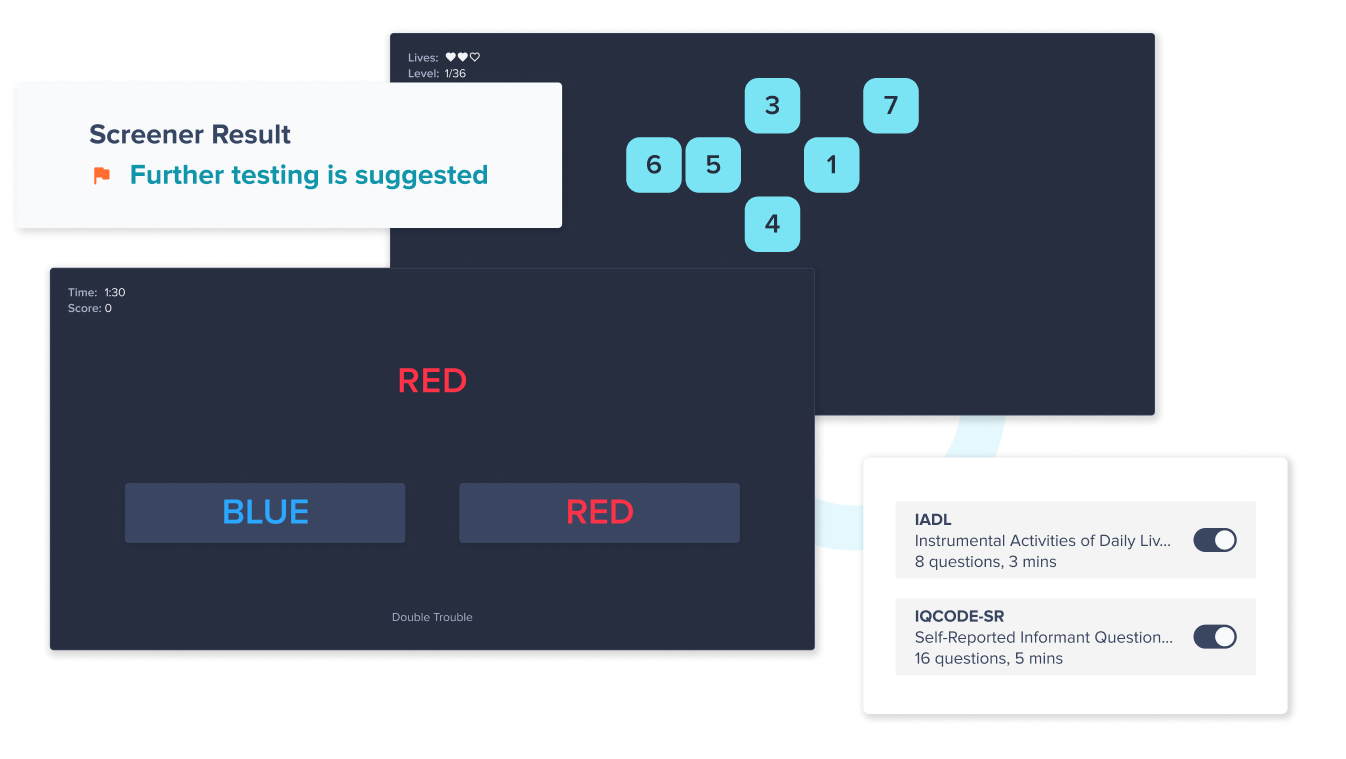
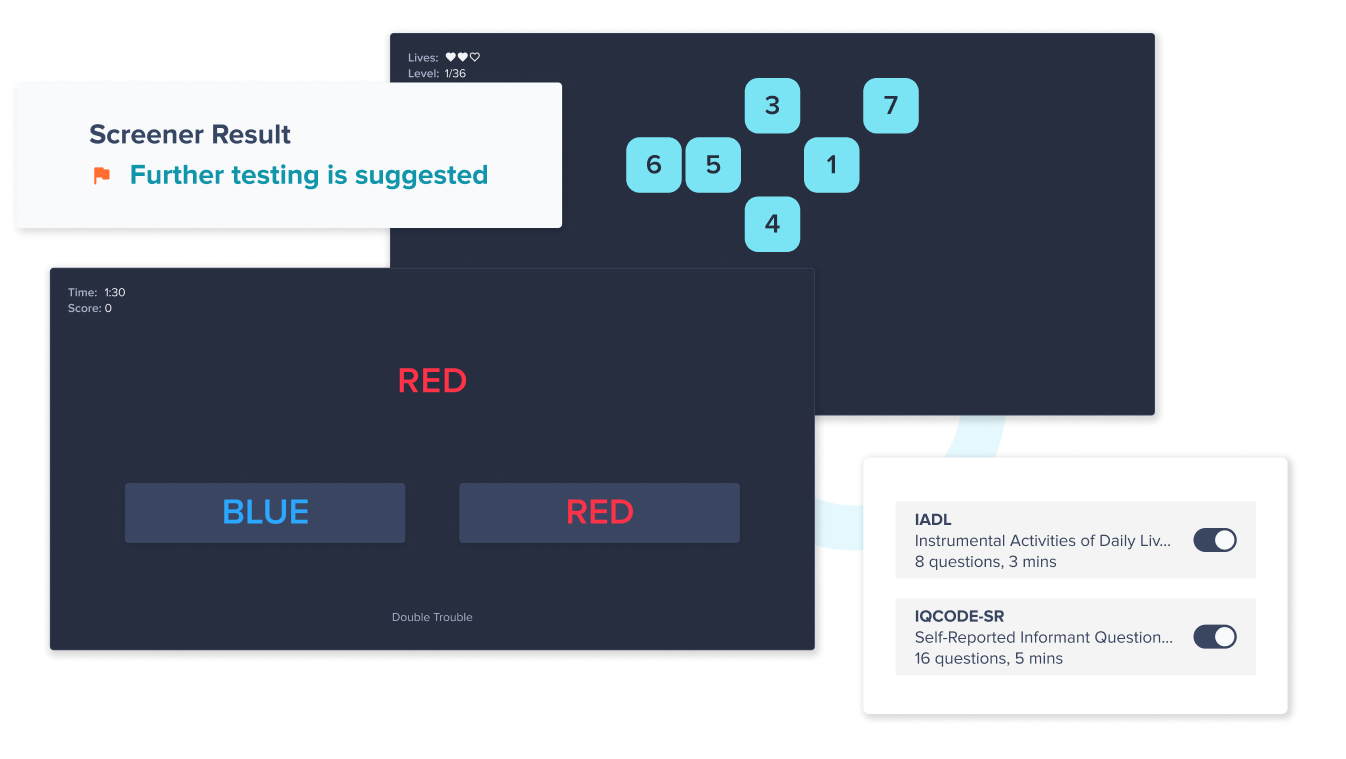
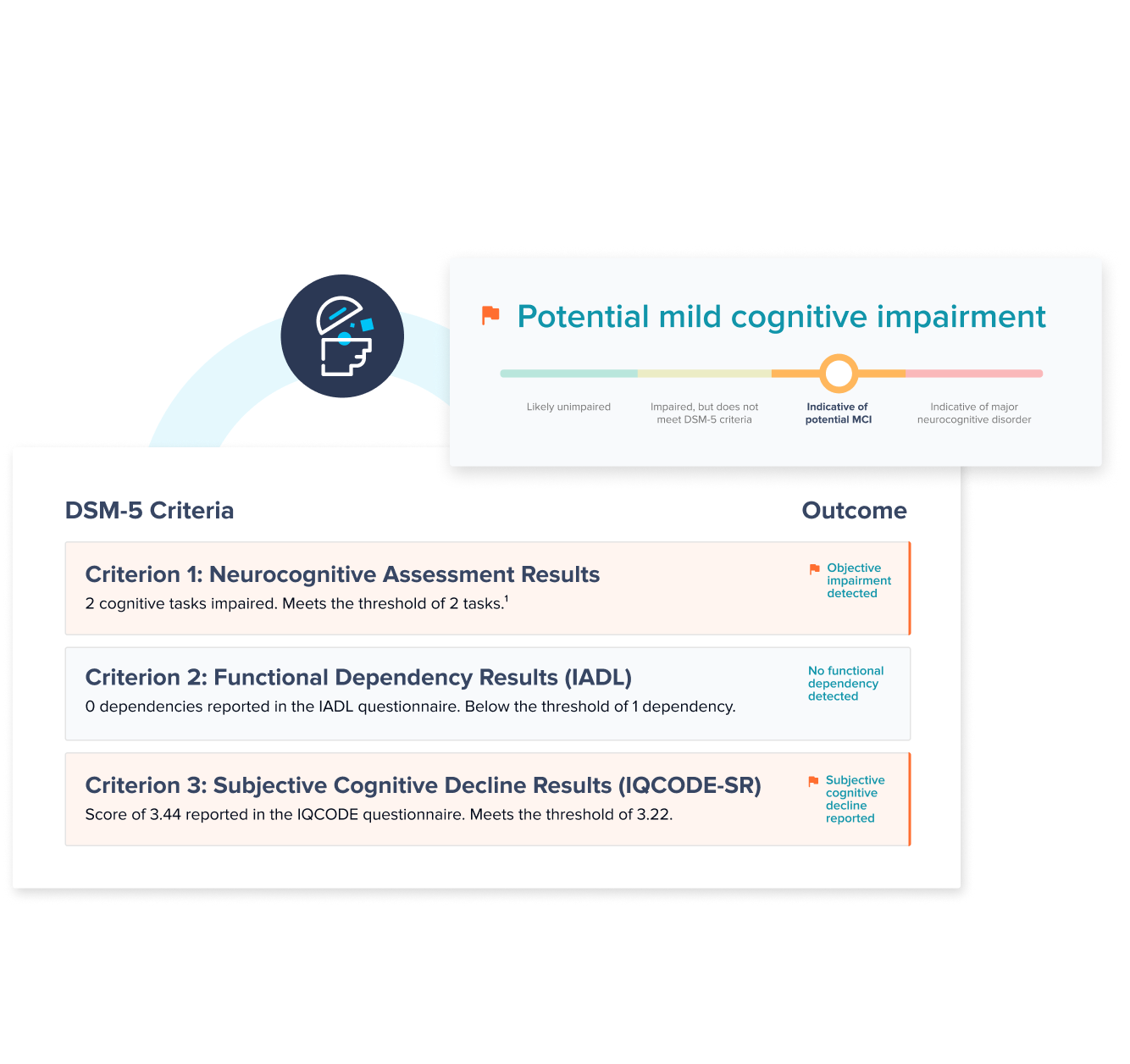
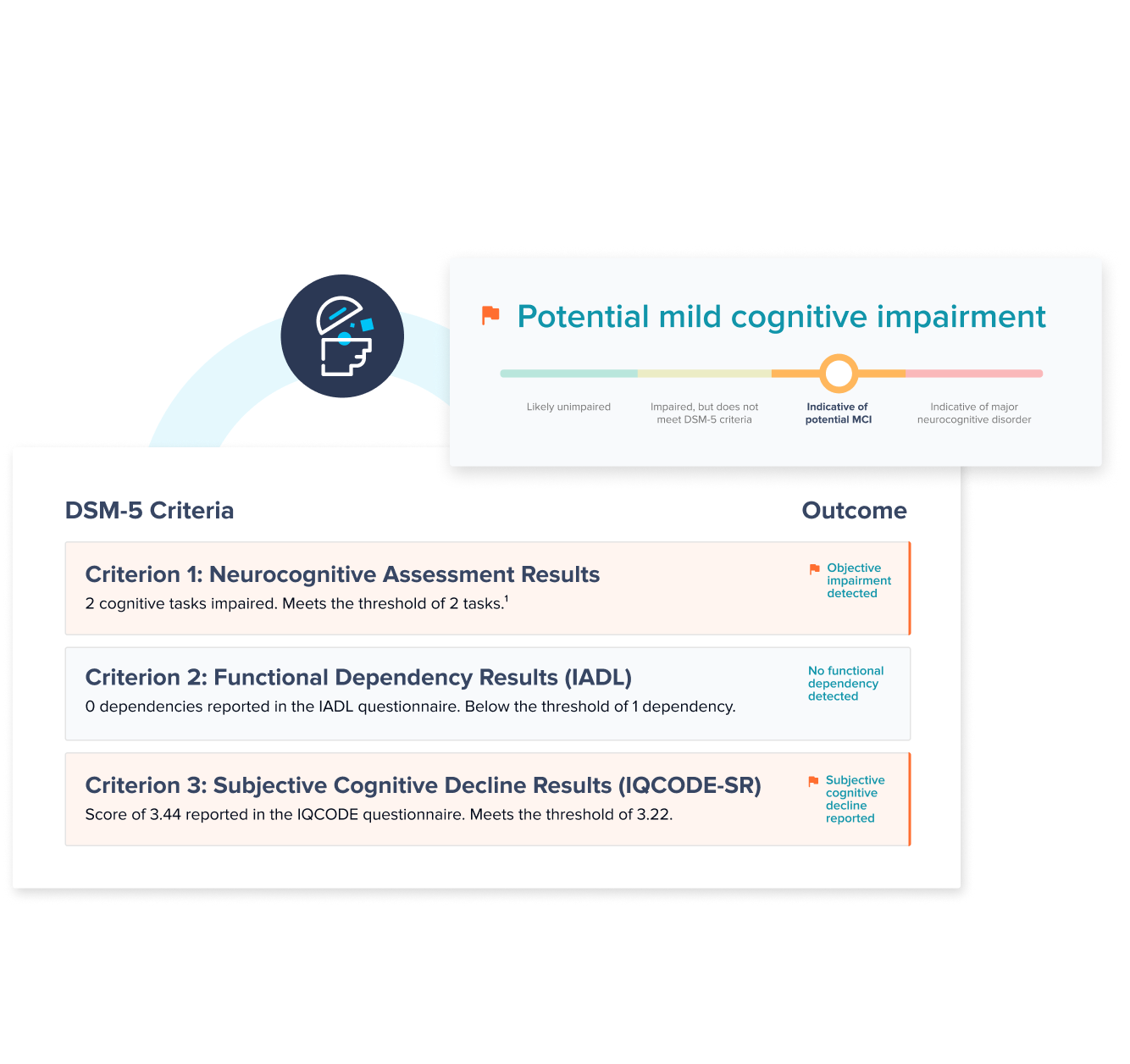
Online screener, assessment, and questionnaires—clinically validated, age-normed, and aligned to DSM-5 diagnostic criteria.

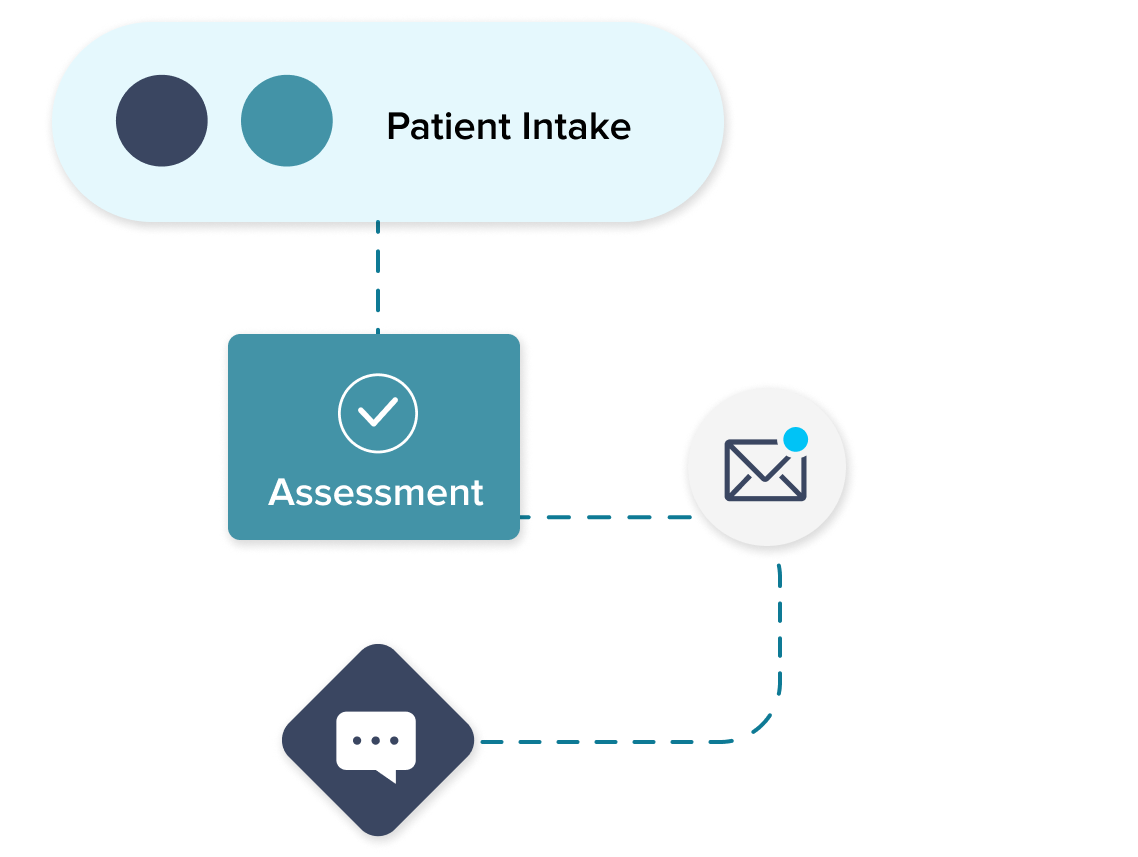
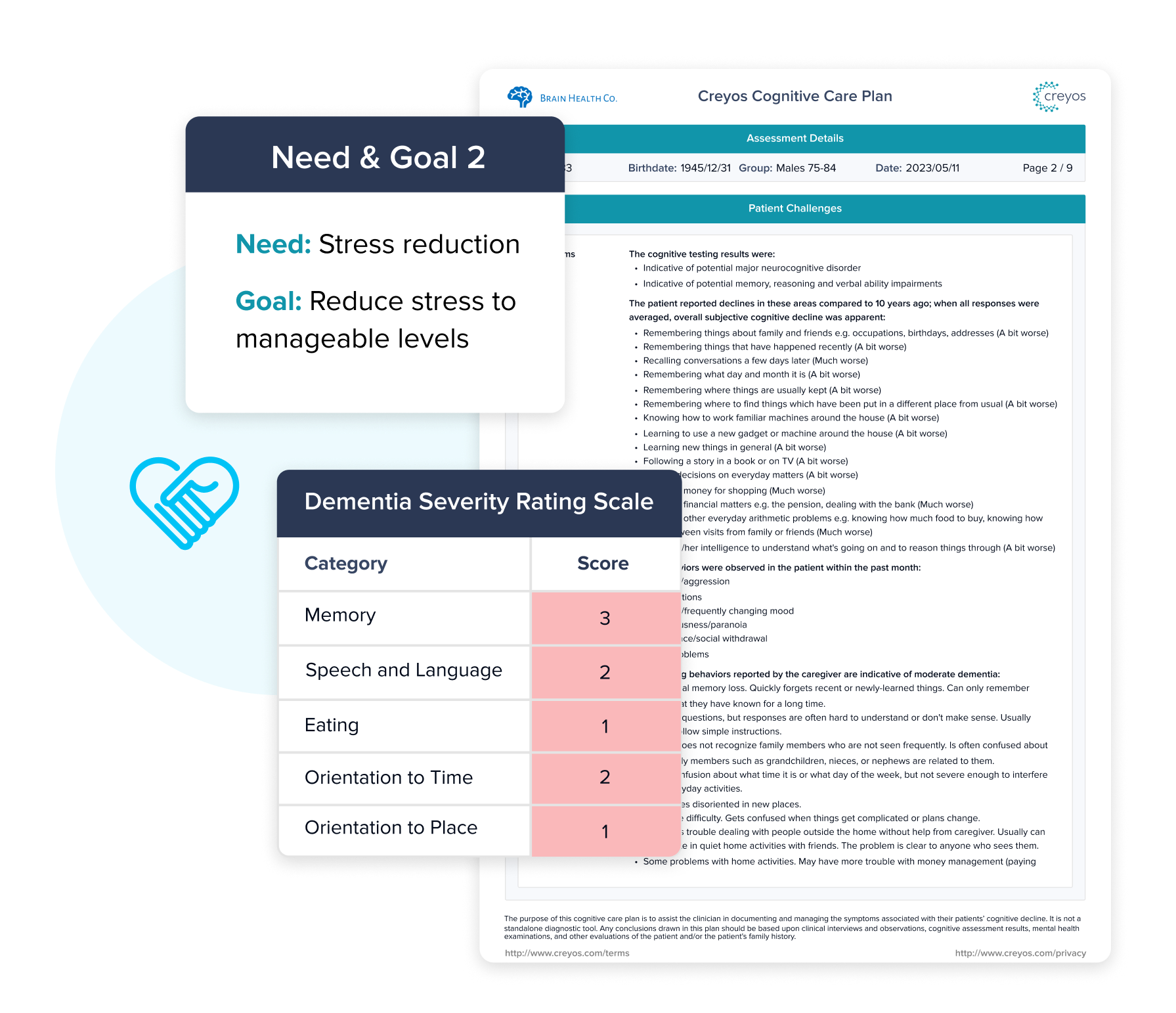
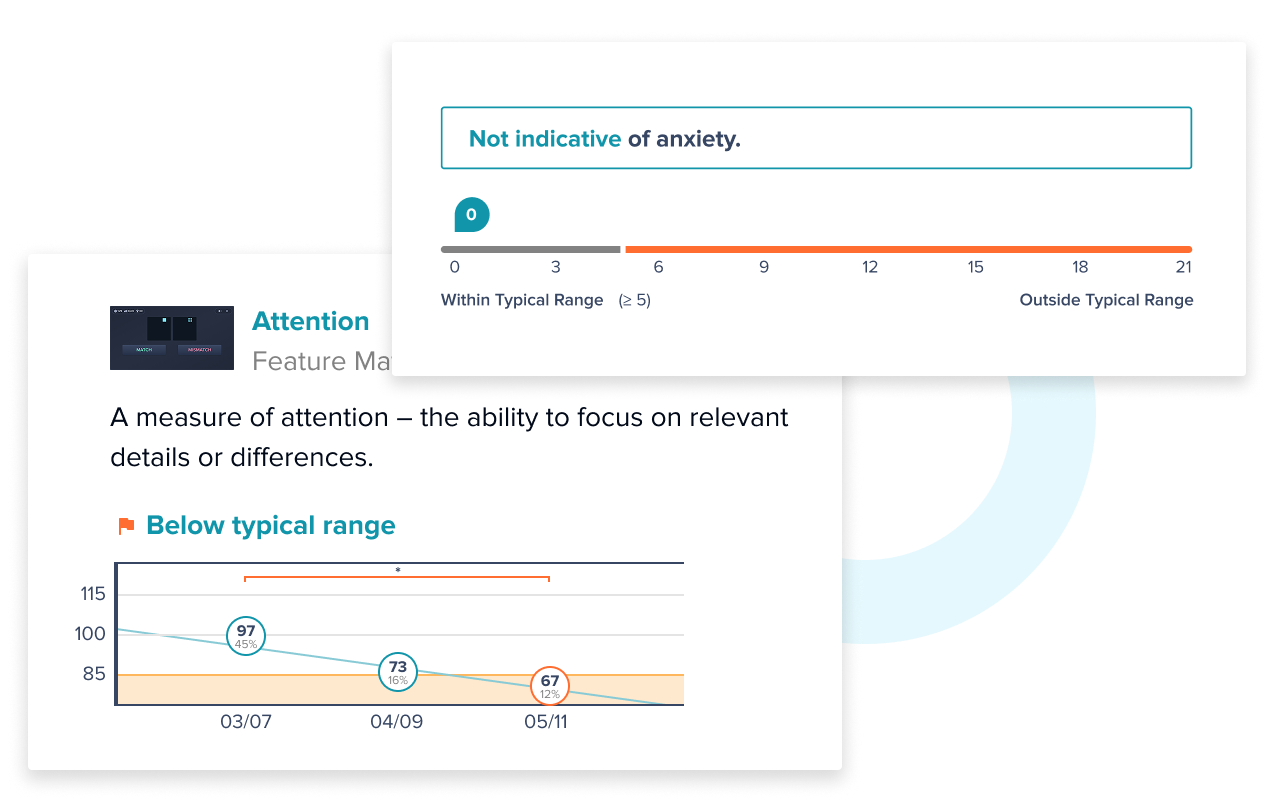
Instant reports with actionable insights to support diagnosis and to drive care pathways and coordinated interventions.

Functions across team-based care models with EHR interoperability, remote testing ability, and no special training required.

Built on rigorous science—35 years of research, an 85,000 participant normative database, and validation in over 400 peer-reviewed studies.
Clinical Outcomes
Value Based Care Impact



Following the COVID-19 pandemic, telehealth implementation...
Read more

Sleep, far from being a passive state of rest, is a dynamic...
Read more

According to a study from the Alzheimer’s Society, over 62%...
Read more
Creyos has been validated as a more scalable and efficient alternative to neuropsychological testing, providing detailed insights into specific cognitive domains in a fraction of the time required for a full neuropsychological battery. Its tasks have demonstrated strong correlations with gold-standard neuropsychological tests, offering high convergent validity and supporting its use as an informative follow-up to initial screening.
Yes—Creyos is specifically designed to detect subtle cognitive changes often missed by screening tools like the MoCA or MMSE. It measures multiple domains, including memory and executive function, to help identify early decline, even if it has not yet affected everyday tasks or responses to simple screeners. A series of recent studies provide compelling support for integrating Creyos assessments into routine cognitive evaluations and leveraging it as an alternative to the MoCA or MMSE.
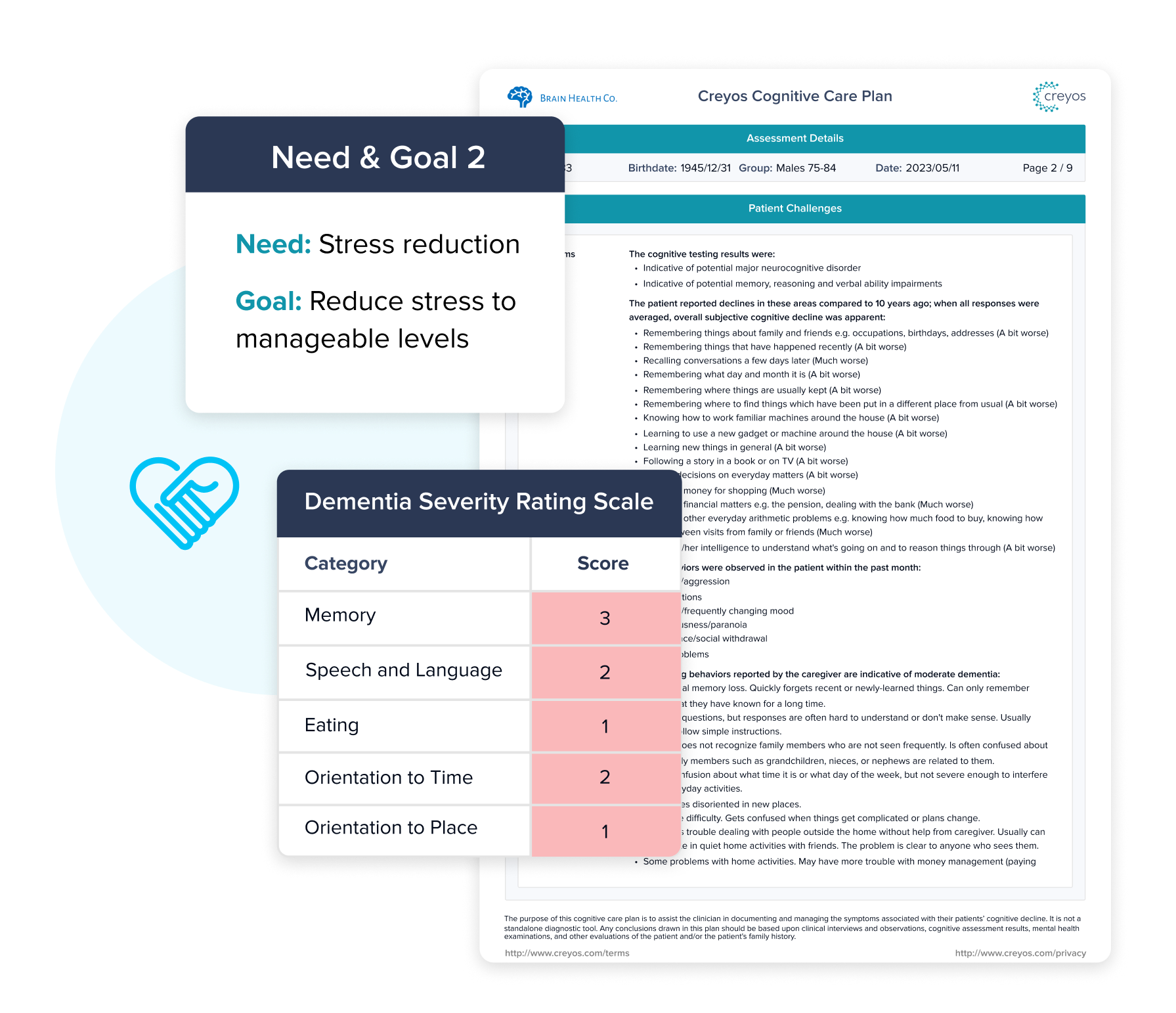
Creyos supports Medicare requirements by streamlining both cognitive assessment and care planning in a single platform. It enables fast, standardized cognitive testing as part of the Annual Wellness Visit (AWV), helping providers efficiently meet documentation requirements while identifying early signs of impairment. This is especially important under CMS-HCC V28, where a timely and accurate dementia diagnosis contributes to appropriate risk adjustment and care management.
Beyond assessment, Creyos offers built-in care plan creation to guide next steps for both the provider and patient. Clinicians use the results from the Creyos dementia assessment to document personalized care plans, including recommendations for follow-up testing, behavioral health support, medication management, caregiver guidance, and lifestyle modifications—ensuring compliance with Medicare expectations, while supporting better outcomes across the care continuum.
Yes. Creyos helps providers identify signs of dementia that traditional screening tools often miss and supports the diagnostic specificity required under CMS-HCC V28.
Using a sensitive, scientifically validated digital screener and assessment, Creyos detects cognitive impairment across a full range of severity—from mild to moderate to severe. This enables earlier identification and more accurate differentiation of dementia stages, which is essential for compliant and specific coding under V28.
Creyos helps health systems detect dementia earlier and more often—typically increasing detection rates from the typical 4-6% to 8-12% of their 65+ patient population. That translates to significantly more patients receiving timely diagnoses and care, and a meaningful financial impact: each additional diagnosis can add roughly $2,400 per member in RAF-adjusted reimbursement annually.
Early detection also leads to better care planning and fewer high cost events. Studies show that people with undiagnosed dementia are up to two times more likely to be hospitalized, and account for up to 40% higher healthcare costs. With Creyos, providers can intervene earlier—reducing preventable hospitalizations and ER visits, all of which lower total cost of care and support quality metrics around screening, care coordination, and chronic condition management.